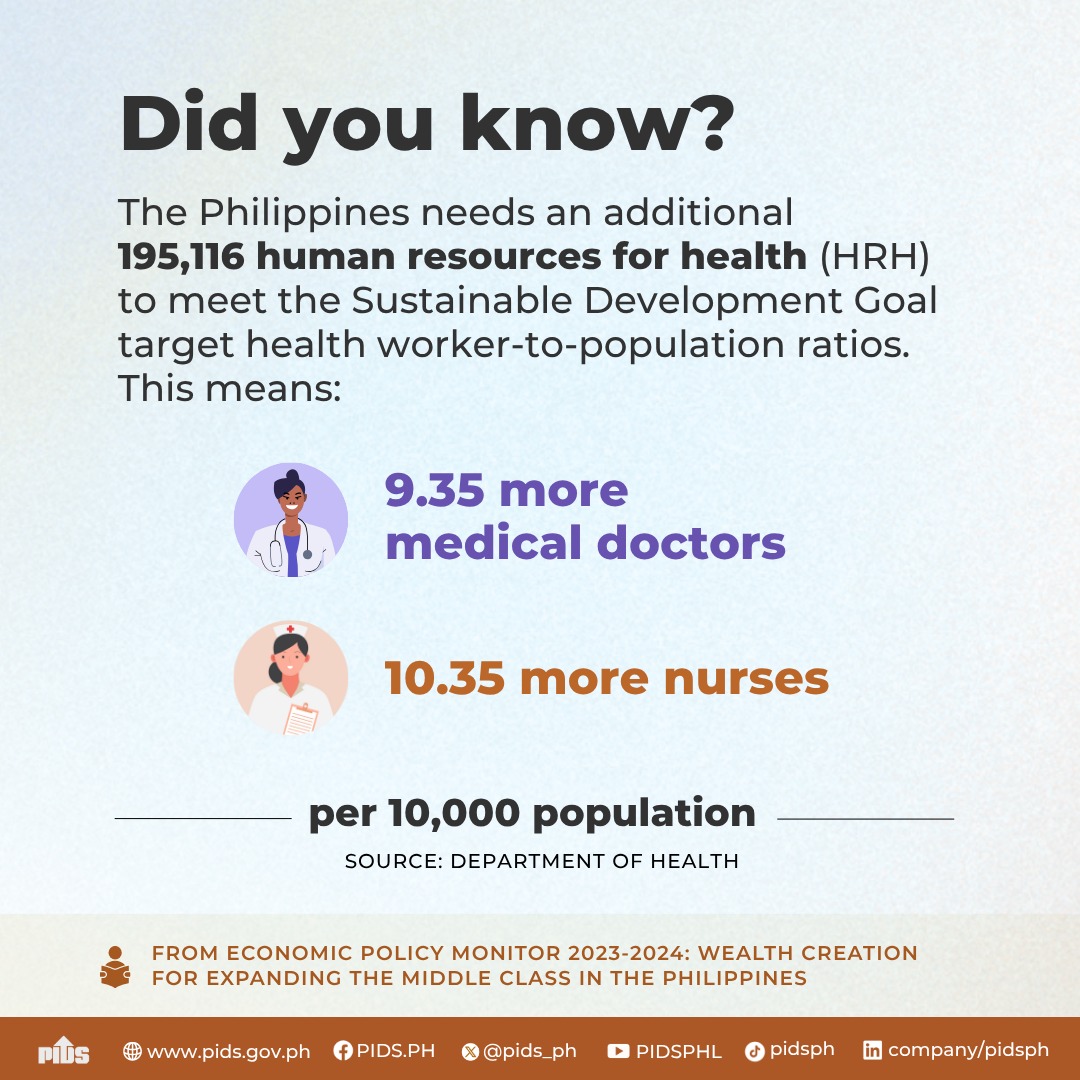
Liberalizing hospital ownership in the country is key to doubling the number of hospital beds within the next two to four decades, according to the state think tank Philippine Institute for Development Studies (PIDS).
In a study, titled Regional Health Integration and Cooperation in the Philippines, PIDS Research Fellow Valerie Gilbert T. Ulep and Research Analyst Lyle Daryll D. Casas said allowing 100 percent foreign hospital ownership would help close the gaps in health infrastructure in the country.
Based on data, Ulep and Casas said, the Philippines, a middle-income country, has one bed per 1,000 population. This rate is similar to most low-income countries in the world.
“The government needs to attract both domestic and foreign investments to help the government in closing health infrastructure gaps in the medium to long term,” Ulep and Casas said.
“Increase equity threshold for hospital foreign investments to 100 percent. The government may want to impose this especially in provinces where there is dire need,” they added.
Apart from this, Ulep and Casas recommended that the government should provide tax breaks for hospital investments for both local and foreign investments, particularly building facilities in provinces.
The authors said the government should also accelerate investment approvals for health infrastructure, services and the purchase of medical equipment.
These steps, the authors said, would help attain the goals set by the 2020-2040 Health Facility Development Plan (HFDP) of the Department of Health (DOH).
The HFDP, therefore, identifies the immense role of the private sector to complement scarce public resources.
Based on the study findings, public spending on health made by the Philippine government is one of the lowest in the Asean region. The authors noted that based on 2018 data, public spending on health was $46 per capita.
This, Ulep and Casas said, is considered low relative to other middle-income countries, such as Thailand, Vietnam, Malaysia, and Indonesia in the region. Thailand and Malaysia spent four times more than the Philippines.
The PIDS researchers also noted that the country’s public spending on health was about 1.5 percent of GDP, significantly lower than Thailand, Vietnam, Singapore and Malaysia.
Singapore spent the most at $1,262 per capita followed by Malaysia, $194 per capita; Thailand, $188 per capita; Vietnam, $65 per capita; and Indonesia, $56 per capita.
“The country’s poor performance in improving health outcomes brought by a number of barriers in the different elements of the health systems infers the need for robust domestic reforms in order to liberalize the country for cross-border health integration,” the researchers said.
Apart from these, the researchers also recommended strengthening the implementation of digital health strategies.
This means developing telemedicine by passing into law the eHealth Systems and Services Bill. Telemedicine is still in its infancy in the Philippines but could provide a means for greater regional integration in terms of health services.
The authors also recommended the development and implementation of a well-thought medical tourism program.
This means identifying a niche in medical tourism. The government can focus on making the country a wellness center, especially for the elderly by offering aging and retirement homes that can help create communities with the ecosystem that promotes health communities.
The authors said the government plans to build a niche in aesthetics, dental service, and wellness services. However, Ulep and Casas said the competition in these areas is tight in the region.
Further, the country should strengthen and complement the establishment of three mutual recognition arrangements (MRAs) that would allow greater mobility of health professionals in the Asean region.
This also means the country should not restrict the practice of health-care providers in the country to Filipino residents.
The MRAs, which allow physicians, nurses, and dentists to physically move freely throughout the Asean region, were designed at a time when these professionals had to be physically present in host countries.
This can already be remedied through the use of technology. The authors said limiting the MRA to the physical presence of professionals in host countries “defeats the purpose of MRAs, which is to harmonize practice across the region.”
“Expert discussions regarding this matter should be initiated, as this could help augment the country’s health system, while establishing regulations to safeguard the public’s safety, which is of utmost importance,” the authors said.
Study pushes liberalization of hospital ownership to boost Philippine health-care system