THE government only spends the cost of a P300-prepaid call card on primary healthcare (PHC) for every Filipino annually, according to state think-tank Philippine Institute for Development Studies (PIDS).
Based on the report titled “Primary Healthcare and Management of non-communicable diseases (NCDs) in the Philippines,” a research team led by PIDS Senior Research Fellow Valerie Gilbert T. Ulep said the low spending on PHC hobbles moves to address the growing threat of NCDs.
The report stated that government only spent $6 or, at the current exchange rate of P50 to the dollar, P300 on PHC services. Countries in the Association of Southeast Asian Nations regions, on average, spend $20 or P1,000 for primary health care.
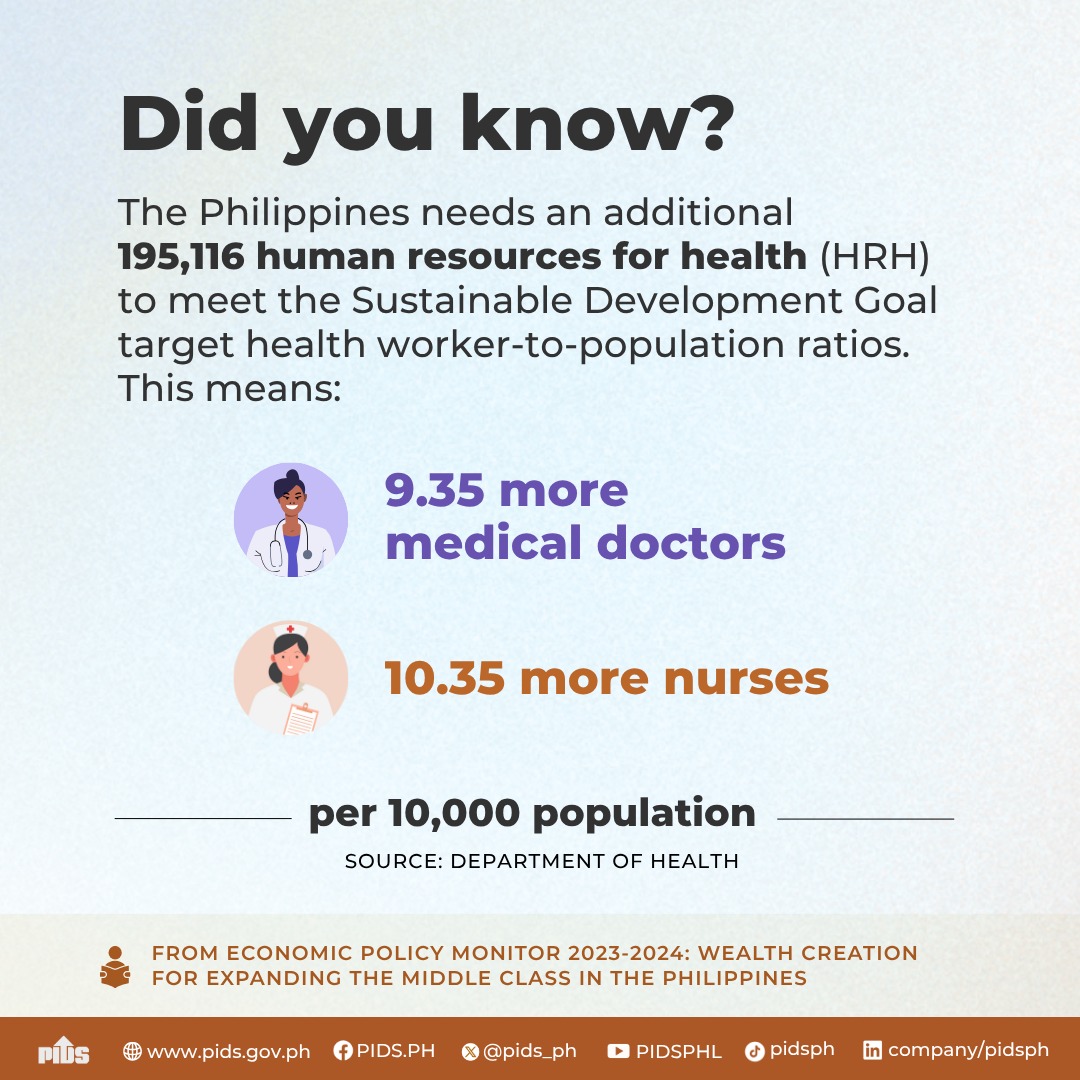
“The large inequalities in health facilities and human resources also suggest the variable capacity of local governments to implement NCD interventions in PHC settings,” the authors said.
“The national government has tried to address this in the past decade by providing grants to augment the capital infrastructure requirement and health human resources of local governments,” they added. “However, these grants do not fully address the supply constraints of LGUs in providing PHC services in communities.”
Causes of death
BASED on the research, the country spent about P640 billion on healthcare. Of this amount, about 40 percent were accounted for by NCDs.
From 2014 to 2018, health spending on NCDs increased to nearly P240 billion in real terms using 2018 prices from P154 billion.
The research also stated that only a small percentage (4 percent) of the country’s health spending was accounted for by PHC facilities.
This is a concern, the authors said, given that NCDs still account for 70 percent of the total deaths in the country and about 65 percent of the disability-adjusted life years (DALYs).
NCDs, they explained, include cancers, chronic respiratory diseases, cardiovascular diseases and diabetes, among others.
Based on the the research, the burden of ischemic heart disease in DALYs increased to 7.5 percent in 2019 from 1.9 percent in 1990.
Other NCDs, such as stroke, LRTI, chronic kidney disease and diabetes, are included in the top 10 burden of diseases in the country.
Preliminary estimates of the Philippine Statistics Authority (PSA) showed that despite the pandemic, NCDs remained to be the top four causes of death in the country.
The data showed that between January and June 2021, the top Filipino killers are: ischaemic heart diseases, which caused the death of 56,757 Filipinos; cerebrovascular diseases, 30,798; neoplasms, 27,343; and, diabetes mellitus, 19,802.
The combined total of these top causes of death in the first six months of the year was 134,698. This figure already represented 44.4 percent of the 303,364 Filipinos who died of various causes during the period.
Increasing faster
CITING latest mortality data from the PSA, the researchers said that NCDs are increasing at a much faster rate in poor communities than in rich ones.
“While the share of NCD deaths among all deaths in the poorest communities was lower than in rich communities, an upward trend over the last decade was observed,” they added.
In order to address the growing threat of NCDs on the population, the authors recommended that a “system-wide and comprehensive health system reform” be implemented.
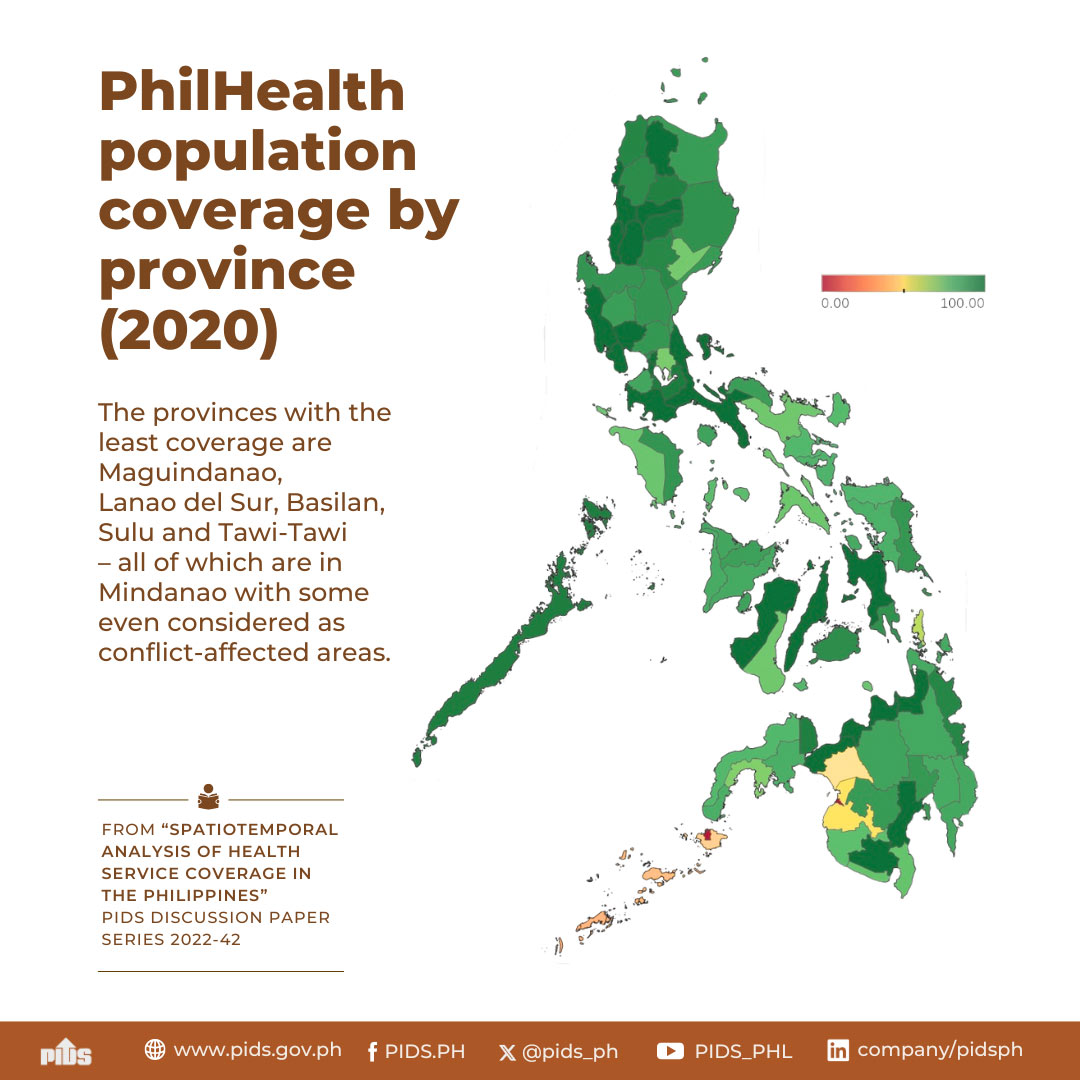
The primary recommendation is to facilitate the implementation of the Universal Healthcare Act, which will expand the breadth and depth of PhilHealth (Philippine Health Insurance Corp.).
The authors also said the UHC will facilitate the integration and referral systems through the creation of province- or city-wide healthcare provider networks (HCPNs).
The researchers said public and private health facilities should be integrated into the network that provides coordinated healthcare services.
“The UHC Act also reinforces sustained capital investments to reduce the huge gap in the health infrastructure of PCFs and health human resources, as envisioned in the ‘Philippine Health Facility Development Plan 2020–2040’ and the ‘National Health Human Resource Masterplan 2020–2040,’” the authors said.
Govt spending on health care equivalent to P300 load–PIDS