POLITICAL Science students would have vivid lessons on public governance as they read besides newspaper opinions, commentaries and remarks from readers on the consequences of devolution following the enactment of Republic Act 7160, otherwise known as the “Local Government Code of 1991.” This was signed into law on Oct. 10, 1991 and took effect on Jan. 1, 1992, 28 years ago. Studies on the devolution have highlighted the importance of “a well-planned and well-designed government policy to minimize, if not avert, unintended consequences; and mainstreaming of health policy reforms to ensure sustainability.” Suggestions include that there be “a closer look at the experience of local government units (LGUs) that were able to reap the benefits of health devolution and find out how the good practices can be replicated in other LGUs.” Practices that have proved negative to good intentions of the law should nonetheless be made known as lessons for governance. Especially due this pandemic the whole world confronts, it is high time there be a “review and assessment of the various health reforms and mechanisms that have been in place to draw lessons and insights that are useful for crafting future health policies.” <https://pidswebs.pids.gov.ph/CDN/PUBLICATIONS/pidsdps1836.pdf>
One such commentary that drives to the point the consequences of health devolution as our country confronts Covid-19 comes from a seasoned multiawarded hospital administrator, Chief of Hospital 3 of the J.R. Borja General Hospital in Cagayan de Oro City, Dr. Ramon M. Nery, MD, FPSP, MHA, CEO 6. Commenting about “The Covid-19 pandemic: ‘An ounce of prevention is better than a pound of cure,’” he wrote:
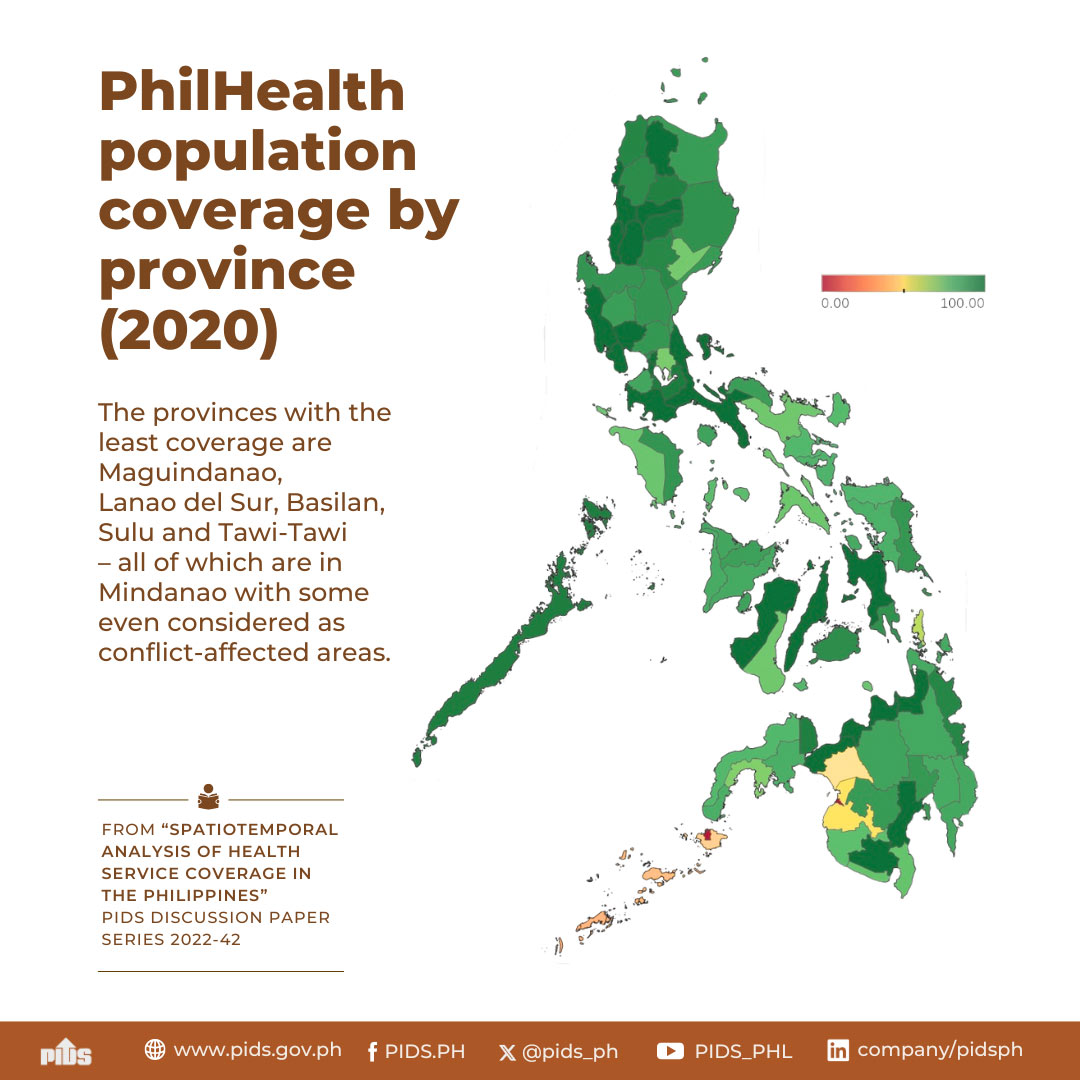
“The Covid-19 pandemic brings to light a fundamental flaw in our health care system — a fragmented structure brought about by devolution in 1991. Under this set up, the Department of Health (DoH) lost its authority and control over the local health facilities now owned, managed, and operated by ill-prepared local government units (LGUs) — compromising availability, access, and quality of much needed curative care services for the poor patients. Public health was likewise in disarray, having no integrated national public health program for LGUs under one office.
“The present pandemic poses a great challenge to our ailing healthcare system. The futile attempts to curb the spread of the virus exposed its inadequacies with LGUSs embarking on their own respective independent response programs. Both national and local response measures and funding mainly focused on curative care and social amelioration while preventive measures were relegated to media issuances, sporadic advocacy campaigns and training, and lately, consultative meetings for selected LGUs. Latest data show a surge in Covid 19 cases rapidly overwhelming our hospitals — a clear consequence of having no concrete comprehensive public health response program against the virus. To date, the Philippines has the highest number of Covid 19 cases in Southeast Asia!
“Statistics show that most Covid-19 cases in the country are clustered in the National Capital Region (NCR), Cebu City, and most highly urbanized cities except for some with functional and well organized public health systems, like Cagayan de Oro City, which despite having one of the highest population densities outside NCR, had one of the the lowest number of cases nationwide. Their strategies, while very tedious, were simple and effective following WHO (World Health Organization) standards.
“The main factor of their success however, anchored mainly on an efficient public health organizational structure under the City Health Office with a team of competent medical and para medical staff , including an army of baranggay (village) health workers and volunteers, the ‘foot soldiers’ with extensive experience from past outbreaks. Full support of the Local Chief Executive, the City Council, and the whole LGU bureaucracy likewise facilitated the implementation of their successful strategic response against the contagion.
“Rather than fixing our fragmented healthcare system at this point, what is urgently needed is to establish a transitory national public health structure separate from the curative care system, akin to the health system in Vietnam (2-track, curative and public health systems), to be headed preferably by an experienced Epidemiologist who will be responsible for the planning, organization, governance and guidance of the Covid-19 response program in the country in coordination with other relevant agencies. This office will have direct lines of authority over the provincial, city, municipal, and baranggay public health facilities (Unity of Command) — harmonizing and maximizing their respective service capabilities. Benchmarking with successful LGUs like Cagayan de Oro City and Baguio could be done to fast track the implementation of strategic imperatives. With this system in place, a more realistic, rational, and cost efficient national preventive public health strategy for the Covid-19 pandemic would have a greater likelihood of success — decongesting our hospitals, saving precious lives and our economy in the process. Public health relegated to the background simply will not work.”
Dr. Nery, a lifetime Fellow of the Philippine Society of Pathologists, a multi-awarded chief executive of a number of hospitals in his 34-year career of public service, was also a 2011 Outstanding Filipino Honoree for Government and Public Service awarded by the JCI Senate Philippines/Insular Life.
Cross our fingers! Let such voices be heard by our lawmakers.
One such commentary that drives to the point the consequences of health devolution as our country confronts Covid-19 comes from a seasoned multiawarded hospital administrator, Chief of Hospital 3 of the J.R. Borja General Hospital in Cagayan de Oro City, Dr. Ramon M. Nery, MD, FPSP, MHA, CEO 6. Commenting about “The Covid-19 pandemic: ‘An ounce of prevention is better than a pound of cure,’” he wrote:
“The Covid-19 pandemic brings to light a fundamental flaw in our health care system — a fragmented structure brought about by devolution in 1991. Under this set up, the Department of Health (DoH) lost its authority and control over the local health facilities now owned, managed, and operated by ill-prepared local government units (LGUs) — compromising availability, access, and quality of much needed curative care services for the poor patients. Public health was likewise in disarray, having no integrated national public health program for LGUs under one office.
“The present pandemic poses a great challenge to our ailing healthcare system. The futile attempts to curb the spread of the virus exposed its inadequacies with LGUSs embarking on their own respective independent response programs. Both national and local response measures and funding mainly focused on curative care and social amelioration while preventive measures were relegated to media issuances, sporadic advocacy campaigns and training, and lately, consultative meetings for selected LGUs. Latest data show a surge in Covid 19 cases rapidly overwhelming our hospitals — a clear consequence of having no concrete comprehensive public health response program against the virus. To date, the Philippines has the highest number of Covid 19 cases in Southeast Asia!
“Statistics show that most Covid-19 cases in the country are clustered in the National Capital Region (NCR), Cebu City, and most highly urbanized cities except for some with functional and well organized public health systems, like Cagayan de Oro City, which despite having one of the highest population densities outside NCR, had one of the the lowest number of cases nationwide. Their strategies, while very tedious, were simple and effective following WHO (World Health Organization) standards.
“The main factor of their success however, anchored mainly on an efficient public health organizational structure under the City Health Office with a team of competent medical and para medical staff , including an army of baranggay (village) health workers and volunteers, the ‘foot soldiers’ with extensive experience from past outbreaks. Full support of the Local Chief Executive, the City Council, and the whole LGU bureaucracy likewise facilitated the implementation of their successful strategic response against the contagion.
“Rather than fixing our fragmented healthcare system at this point, what is urgently needed is to establish a transitory national public health structure separate from the curative care system, akin to the health system in Vietnam (2-track, curative and public health systems), to be headed preferably by an experienced Epidemiologist who will be responsible for the planning, organization, governance and guidance of the Covid-19 response program in the country in coordination with other relevant agencies. This office will have direct lines of authority over the provincial, city, municipal, and baranggay public health facilities (Unity of Command) — harmonizing and maximizing their respective service capabilities. Benchmarking with successful LGUs like Cagayan de Oro City and Baguio could be done to fast track the implementation of strategic imperatives. With this system in place, a more realistic, rational, and cost efficient national preventive public health strategy for the Covid-19 pandemic would have a greater likelihood of success — decongesting our hospitals, saving precious lives and our economy in the process. Public health relegated to the background simply will not work.”
Dr. Nery, a lifetime Fellow of the Philippine Society of Pathologists, a multi-awarded chief executive of a number of hospitals in his 34-year career of public service, was also a 2011 Outstanding Filipino Honoree for Government and Public Service awarded by the JCI Senate Philippines/Insular Life.
Cross our fingers! Let such voices be heard by our lawmakers.