One of the more important lessons COVID-19 taught us is the need for more health frontliners, specially outside the main cities. The other lesson is to show appreciation to our frontliners through better pay.
It is also inexcusable that the Department of Health (DOH) was totally unprepared for the epidemic. There was not enough of the personal protective equipment (PPEs), including simple face masks. As a result, so many of our doctors and nurses died unnecessarily in the first few months.
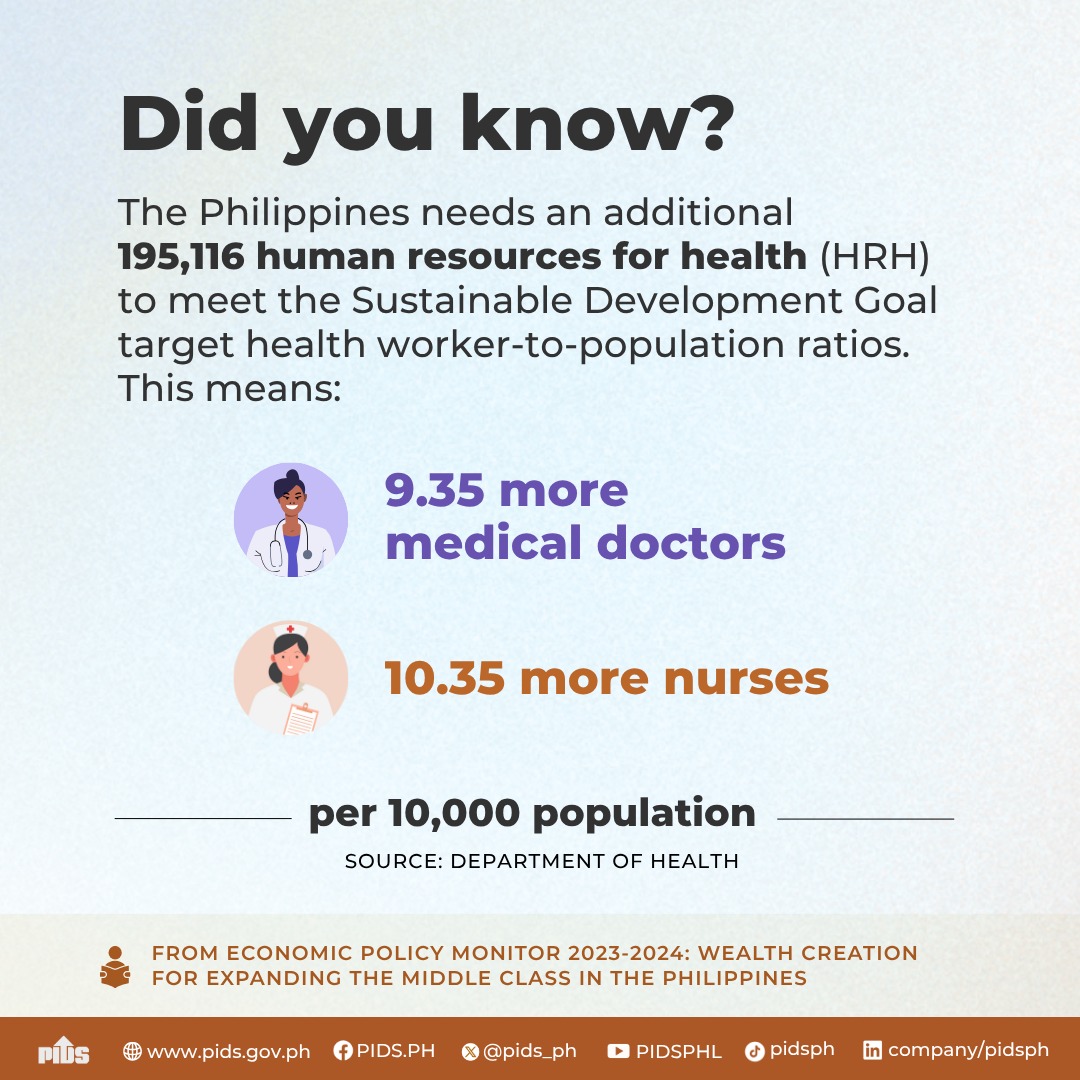
With the COVID-19 pandemic, it became very obvious we didn’t have enough doctors and nurses in active duty in hospitals to take in an avalanche of patients specially outside of NCR. That has always been a problem ignored.
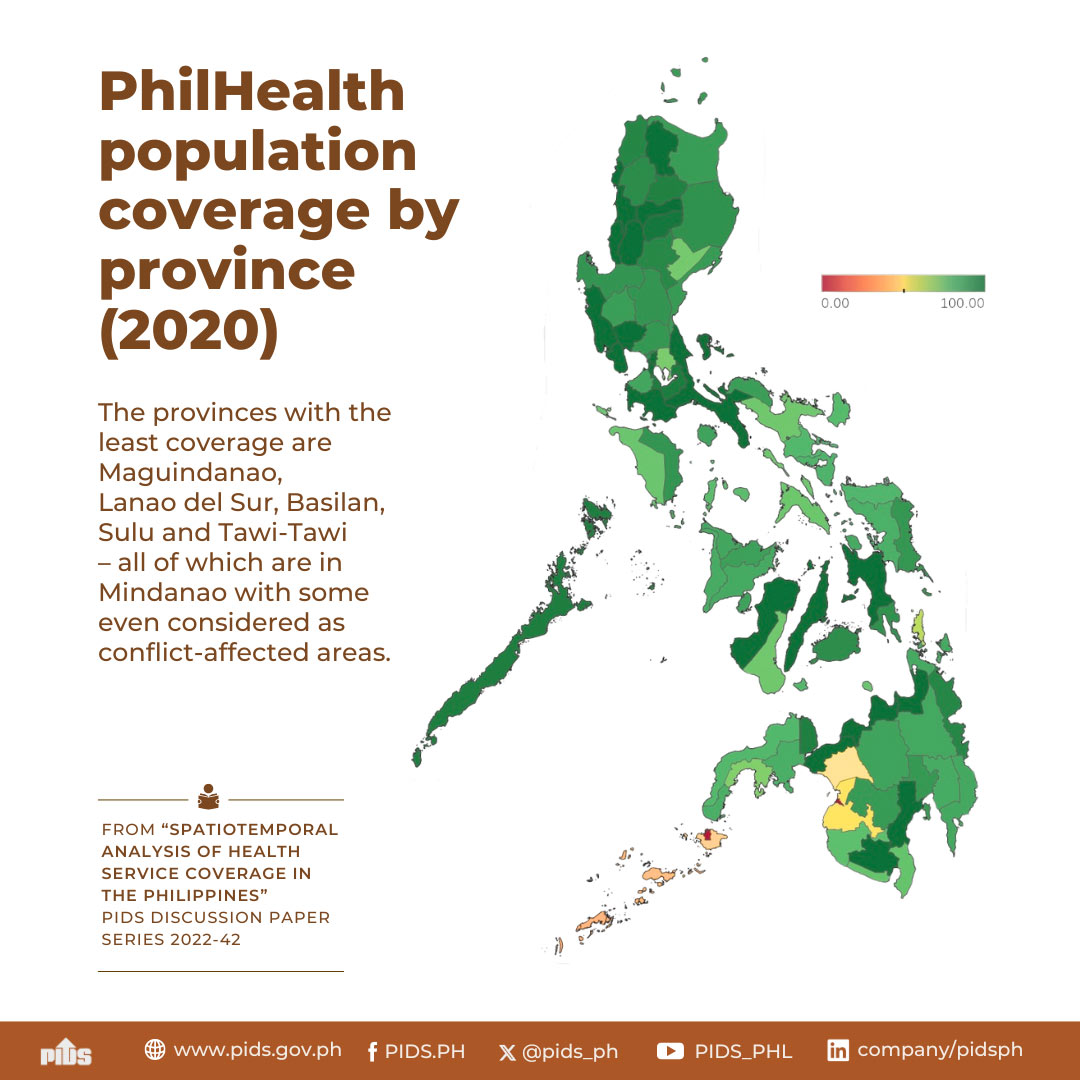
According to a study by government think tank Philippine Institute for Development Studies (PIDS), about 75 percent of cities and towns in the Philippines lack health workers.
“The continuing maldistribution of healthcare workers can aggravate the country’s problem of limited access to healthcare services,” a PIDS research study observed.
Filipino physicians, professional nurses, and professional midwives are more likely to work in areas where earnings are potentially high and near communities where they were trained.
“Less than 25 percent of cities and municipalities have HHR (human health resource) density above the 41 physicians, nurses and midwives per 10,000 population recommended by the WHO (in 2016). This leaves as much as three-quarters of cities and municipalities in the country with potentially insufficient number of HHRs to provide healthcare services,” PIDS explained.
A good number, specially nurses, have gone abroad or have taken non-nursing jobs at home.
What should be done?
One suggestion is obvious: Boost the incomes of healthcare workers to encourage them to stay. The government ban on the deployment of health care workers abroad during the pandemic was wrong. It didn’t get them to help with the pandemic as the President had hoped.
DOH admits only a handful responded to its job offers. Government should have allowed those with foreign contracts to leave, and then convince thousands of nurses who reside here, but who would rather work at call centers for better pay, to work for the DOH.
The bigger problem is simple: Government doesn’t have the infrastructure of hospitals in key regions, largely because we have not invested enough in them through the years.
And it doesn’t seem the government is ready to invest in having hospitals with the caliber of PGH in every region. Looking at the 2021 national budget pending in Congress, there are no allocations to improve our health infrastructure.
There are plans to build permanent evacuation centers. Maybe, they can design these centers to include a medical clinic that can be useful even in ordinary times, if properly funded and staffed.
Actually, there is a better way. Sen. Sonny Angara has filed Senate Bill 1850, or the proposed Healthcare Facility Augmentation Act. Sen. Sonny wants to establish a hospital in every state university and college offering a medical program.
“We need to strengthen our healthcare system and two of the initial steps that we can take is to produce more doctors and nurses, and to increase the number of hospitals that will serve our people,” Angara said.
The other big problem in our healthcare delivery infrastructure is the decentralization of health services. LGUs now have greater responsibility to provide health services and to operate and maintain health facilities such as district hospitals and rural health units.
“Health devolution was supposed to increase LGU spending on healthcare delivery services to achieve better health outcomes. However, this has not been the case in most LGUs… the internal revenue allotment (IRA) of many LGUs is insufficient to finance the operations of devolved hospitals, pay the salaries of health workers, and procure hospital beds and other health supplies,” according to the PIDS study.
But in the end, we go back to lack of staff. We need to start training doctors who will be general practitioners, primary care physicians, and willing to serve outside the big cities.
According to Sen Ralph Recto, a bill providing for medical scholarships is ready for approval by President Duterte. But it must be properly funded.
Sen. Recto complains that Malacañang proposed to halve this year’s P167 million financial subsidies to 1,789 medical scholars to P83.5 million next year. Worse, this year’s P167 million financial stipends to medical students in eight state universities has been impounded “for later release,” Recto said.
The medical scholarship program in eight SUCs is one of the tracks in the Congress–approved bill. It aims to produce doctors whose services are needed in the provinces. Only 25 out of 81 have enough public doctors, Recto said.
Another program is run by the DOH, which had 1,142 scholars in various medical schools last year. Under their contract, they shall “repay” their state-granted tuition and allowances by serving in rural areas after passing the board examinations.
In the meantime, how do we serve the underserved?
PIDS recommend the use of technology as an alternative mode of service. Telemedicine has potential usefulness, but only after DICT has improved broadband connectivity in the countryside.
Another possibility PIDS suggested is certifying some primary healthcare skills that may be done by other types of medical professionals apart from doctors. Even in major metro areas in the US, they are using physicians’ assistants and nurse practitioners to augment the need for health workers to respond to basic needs.
Sen. Recto proposed to name the medical scholarship after the late health Secretary Juan Flavier, famously known as the doctor to the barrios.
Also mentioned was the late Dr. Bobby de la Paz, a UP-PGH trained doctor who left a potentially lucrative big city practice for Samar, where he ran primary health care programs. He was assassinated inside his Catbalogan clinic in April 1982.
Two things we must prioritize to survive this and future epidemics: Having more doctors and nurses serving in the countryside and having a national health infrastructure that can handle all health needs, including pandemics.