The health of Filipinos has significantly improved over the last 50 years. However, many challenges still remain for the health sector to effect further health gains.
Infant and maternal mortality rates in the Philippines remained high in the last decade compared to that of the other ASEAN countries. In addition, the threat from infectious diseases and the burden of degenerative conditions have also been rising. On top of these, emerging health problems brought about by environmental and work-related factors also remain unattended.
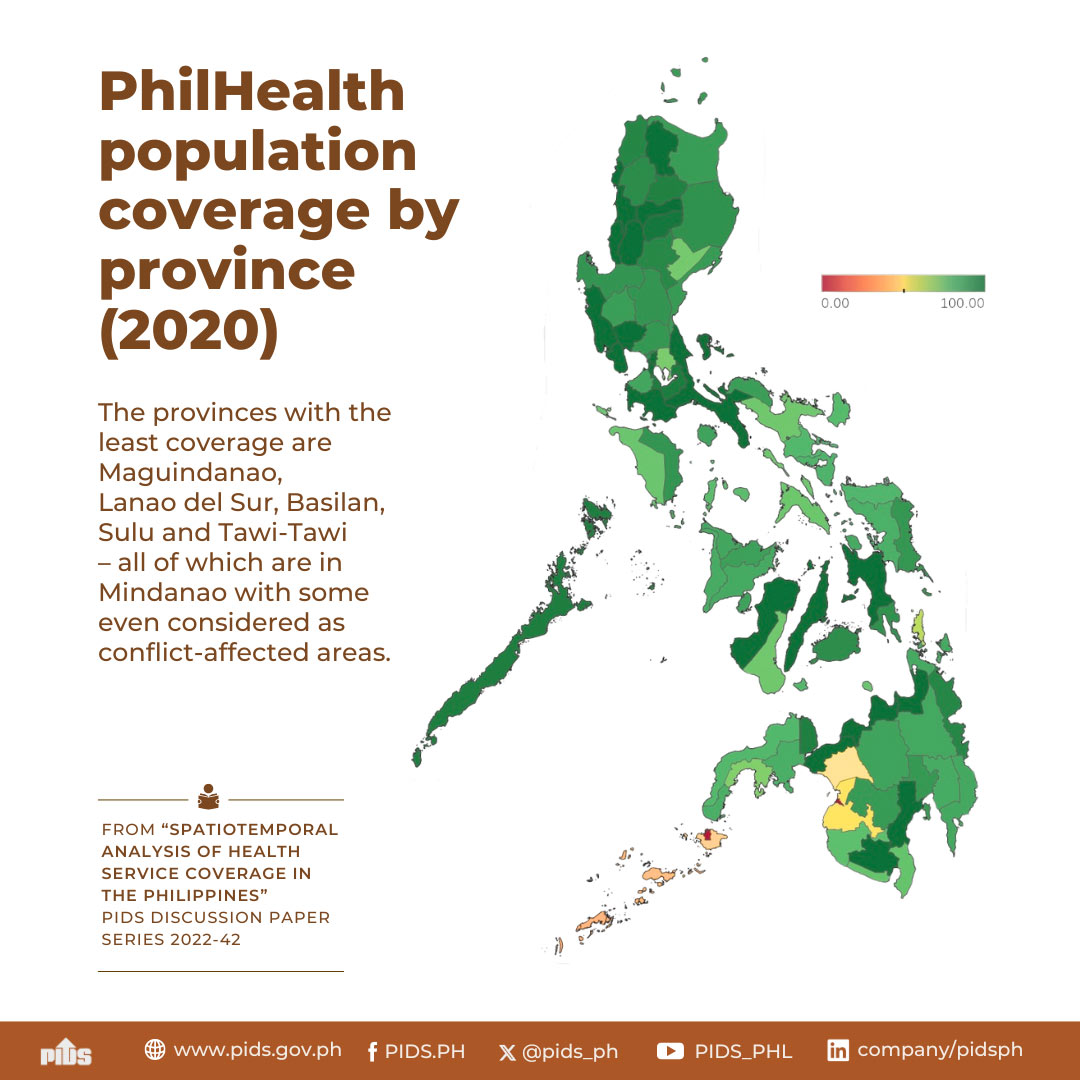
There is also the large variation in health status across population groups, income classes and geographic areas. Those who live in rural and isolated communities receive less and lower quality health services. Even in places where facilities are present, people are unable to receive appropriate care because services are unaffordable. While quality of healthcare is wanting in most areas, costs continue to rise, putting appropriate care beyond the reach of ordinary people. For the poorest of the poor, this means dying without even seeing a doctor.
To address these problems, the agenda for health sector reforms have been developed by the Department of Health (DOH). The Health Sector Reform Agenda (HSRA) describes the policies, public investments, and organizational changes needed to improve the way health care is delivered, regulated, and financed in the country.
Specifically, the HSRA seeks to undertake the following:
Provide fiscal autonomy to government hospitals . The conversion of government hospitals into corporate entities will promote fiscal autonomy by allowing them to collect socialized user fees. This move will take a great chunk off the DOH's yearly appropriation for hospital operations. Thus, the DOH could use this savings to finance preventive public health programs. However, there is a need to enhance the capacities of government hospitals such as their diagnostic equipment, laboratory and medical staff to effectively exercise fiscal autonomy. Such investment must be cognizant of complimentary capacity provided by public-private networks. Most importantly, safety measures shall be carefully put into place to protect the interest of the indigents such as enrolling them in the National Health Insurance Program.
Secure funding for priority public health programs. Budget on a multi-year basis must be provided to eliminate or significantly reduce the incidence of infectious diseases. The government should also allocate funds to effectively address emerging health concerns and to advance health promotion and prevention programs. At the same time, the management capacity and infrastructure of public health programs must be upgraded to ensure that these investments are effectively utilized. Capacity building is likewise required for these programs to provide technical leadership over local health systems.
Promote the development of local health systems and ensure their effective performance. Local government units must enter into cooperative and cost-sharing arrangements to improve local health services. Funds must be secured to upgrade local health facilities and build local human resource capacities. For more effective performance, participation of the private sector and volunteer groups must also be tapped. Lastly, appropriate mechanisms for sustainability and continued delivery of quality care must be developed and institutionalized.
Strengthen the capacities of health regulatory agencies. Health regulatory agencies, namely, the Bureau of Food and Drug (BFAD), the Bureau of Health Devices and Technology (BHDT), the Bureau of Health Facilities and Services (BHFS), and the Bureau of Quarantine and International Health Surveillance (BQIHS) must be strengthened to ensure the safety, quality, accessibility and affordability of health services and products. Public investments must be made to upgrade the facilities and manpower capability of these agencies, particularly in standards development, technology assessment and enforcement. To achieve all these, amendments to the laws governing these agencies are called for.
Expand the coverage of the National Health Insurance Program (NHIP) . Social health insurance must be expanded to widen its reach. Health insurance benefits must be improved to make the program more attractive to members. As membership expands and benefit spending increases, appropriate mechanisms to ensure quality and cost effective services must be developed and introduced. Capacities and new administrative structures must also be developed to allow the Philippine Health Insurance Corporation (PhilHealth) to effectively service more members and manage increased benefit spending.
These five reform areas are highly interdependent, complementary and therefore should be implemented as a package. Health financing reforms through NHIP expansion will make hospital autonomy viable and will ensure that the poor remains protected. Hospital reforms, in turn will free up resources for investments in public health program, and health regulation at the national and local levels. Effective public health programs and local health systems will relieve the NHIP from paying for hospitalizations that should otherwise have been prevented or better handled at primary care facilities.
Implementation of the HSRA demands public investments, policy and organizational changes. The HSRA will require public investments estimated to amount to P112 billion within a five-year period. It will also require effective implementation of existing laws and policies like the National Health Insurance Act, the National Drug Policy and the Local Government Code. The organizational changes needed include the continuing re-engineering of the DOH and PhilHealth and the formation of inter-local health zones.
Ultimately, HSRA aims to: improve the health status of the people through greater and more effective coverage of national and local public health programs; increase access to health services especially by the poor; and reduce financial burden on individual families. It shall be the catalyst that will bring the country toward the realization of a shared vision of health for all Filipinos.
Infant and maternal mortality rates in the Philippines remained high in the last decade compared to that of the other ASEAN countries. In addition, the threat from infectious diseases and the burden of degenerative conditions have also been rising. On top of these, emerging health problems brought about by environmental and work-related factors also remain unattended.
There is also the large variation in health status across population groups, income classes and geographic areas. Those who live in rural and isolated communities receive less and lower quality health services. Even in places where facilities are present, people are unable to receive appropriate care because services are unaffordable. While quality of healthcare is wanting in most areas, costs continue to rise, putting appropriate care beyond the reach of ordinary people. For the poorest of the poor, this means dying without even seeing a doctor.
To address these problems, the agenda for health sector reforms have been developed by the Department of Health (DOH). The Health Sector Reform Agenda (HSRA) describes the policies, public investments, and organizational changes needed to improve the way health care is delivered, regulated, and financed in the country.
Specifically, the HSRA seeks to undertake the following:
Provide fiscal autonomy to government hospitals . The conversion of government hospitals into corporate entities will promote fiscal autonomy by allowing them to collect socialized user fees. This move will take a great chunk off the DOH's yearly appropriation for hospital operations. Thus, the DOH could use this savings to finance preventive public health programs. However, there is a need to enhance the capacities of government hospitals such as their diagnostic equipment, laboratory and medical staff to effectively exercise fiscal autonomy. Such investment must be cognizant of complimentary capacity provided by public-private networks. Most importantly, safety measures shall be carefully put into place to protect the interest of the indigents such as enrolling them in the National Health Insurance Program.
Secure funding for priority public health programs. Budget on a multi-year basis must be provided to eliminate or significantly reduce the incidence of infectious diseases. The government should also allocate funds to effectively address emerging health concerns and to advance health promotion and prevention programs. At the same time, the management capacity and infrastructure of public health programs must be upgraded to ensure that these investments are effectively utilized. Capacity building is likewise required for these programs to provide technical leadership over local health systems.
Promote the development of local health systems and ensure their effective performance. Local government units must enter into cooperative and cost-sharing arrangements to improve local health services. Funds must be secured to upgrade local health facilities and build local human resource capacities. For more effective performance, participation of the private sector and volunteer groups must also be tapped. Lastly, appropriate mechanisms for sustainability and continued delivery of quality care must be developed and institutionalized.
Strengthen the capacities of health regulatory agencies. Health regulatory agencies, namely, the Bureau of Food and Drug (BFAD), the Bureau of Health Devices and Technology (BHDT), the Bureau of Health Facilities and Services (BHFS), and the Bureau of Quarantine and International Health Surveillance (BQIHS) must be strengthened to ensure the safety, quality, accessibility and affordability of health services and products. Public investments must be made to upgrade the facilities and manpower capability of these agencies, particularly in standards development, technology assessment and enforcement. To achieve all these, amendments to the laws governing these agencies are called for.
Expand the coverage of the National Health Insurance Program (NHIP) . Social health insurance must be expanded to widen its reach. Health insurance benefits must be improved to make the program more attractive to members. As membership expands and benefit spending increases, appropriate mechanisms to ensure quality and cost effective services must be developed and introduced. Capacities and new administrative structures must also be developed to allow the Philippine Health Insurance Corporation (PhilHealth) to effectively service more members and manage increased benefit spending.
These five reform areas are highly interdependent, complementary and therefore should be implemented as a package. Health financing reforms through NHIP expansion will make hospital autonomy viable and will ensure that the poor remains protected. Hospital reforms, in turn will free up resources for investments in public health program, and health regulation at the national and local levels. Effective public health programs and local health systems will relieve the NHIP from paying for hospitalizations that should otherwise have been prevented or better handled at primary care facilities.
Implementation of the HSRA demands public investments, policy and organizational changes. The HSRA will require public investments estimated to amount to P112 billion within a five-year period. It will also require effective implementation of existing laws and policies like the National Health Insurance Act, the National Drug Policy and the Local Government Code. The organizational changes needed include the continuing re-engineering of the DOH and PhilHealth and the formation of inter-local health zones.
Ultimately, HSRA aims to: improve the health status of the people through greater and more effective coverage of national and local public health programs; increase access to health services especially by the poor; and reduce financial burden on individual families. It shall be the catalyst that will bring the country toward the realization of a shared vision of health for all Filipinos.