MANILA – Hospitals must adopt certain measures to improve the quality of health care system in the country, according to the latest studies by the government think tank Philippine Institute for Development Studies (PIDS).
"Clearly, it is not enough to improve the accessibility of health services… in developing countries like the Philippines health care access has increased, but health outcomes barely improved. Studies say that one factor contributing to this health care is quality," PIDS Head Aniceto Orbeta Jr. said Thursday.
"COVID-19 pandemic has exposed these issues and further weakened the country’s frail health care system. This public health crisis serves as a reminder that access to affordable and high quality health care is a fundamental human right," Orbeta said.
PIDS believe there are reasons why health care quality should be improved.
"One, as income grows, we are moving towards an upper- middle income country… people will demand for more quality care. So there is a political decision that we need to take to improve on quality. Second, the UHC law outlines the need to improve quality of care.. and how we achieve it. Third, there is a growing use of compliance and value- based financing. Meaning, the use of financing through for example insurance system, to demand quality of care," Dr. Valerie Gilbert Ulep, Senior Research Fellow PIDS said.
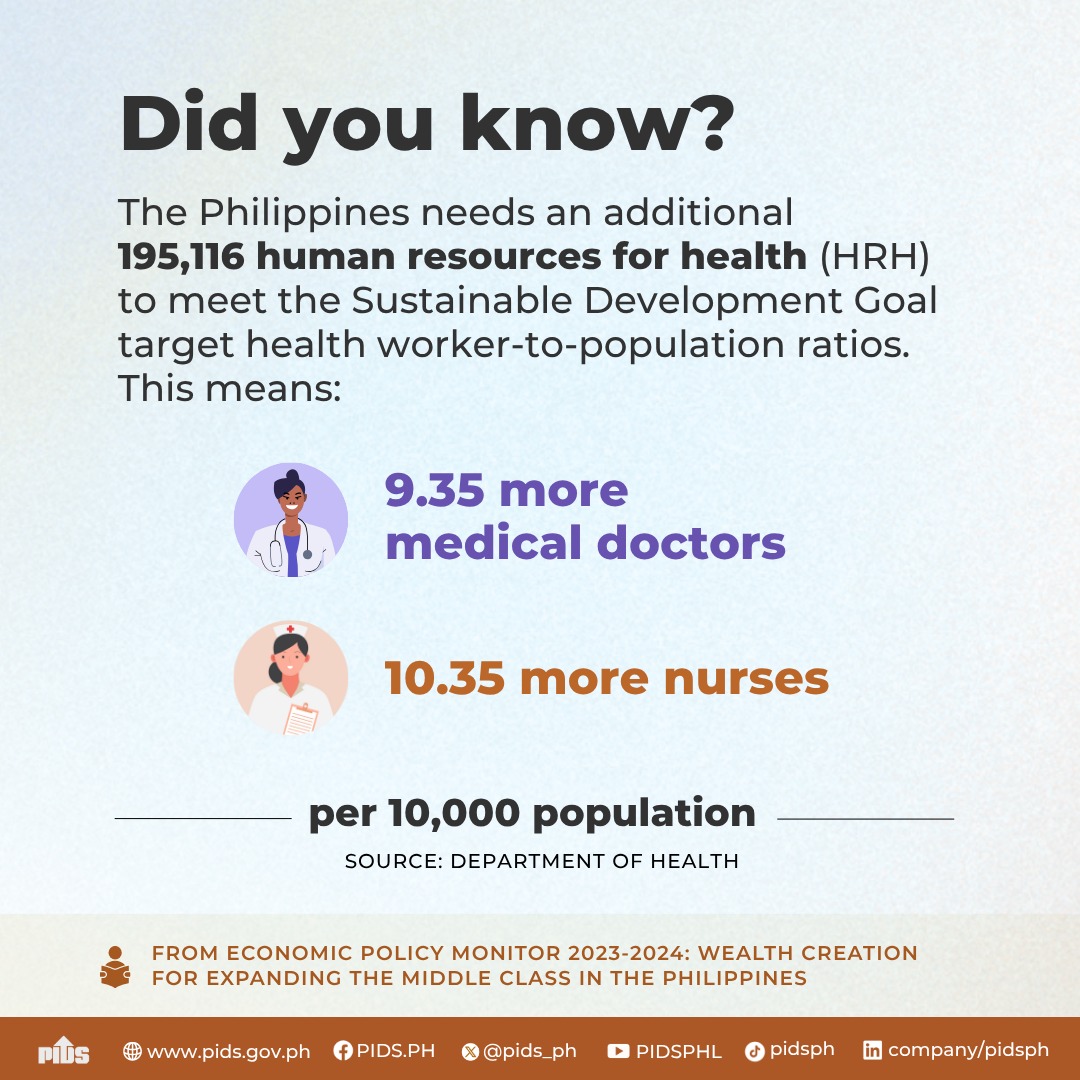
Based on two PIDS studies, there are large gaps that need to be filled before health care quality improves.
FIRST STUDY
The first PIDS study titled "Assessment of Capability and Readiness of Philippine Hospitals to Provide High Quality Health Care" rolled out questionnaires to 469 out of 1,300 licensed hospitals asking about management, human resources for health, basic infrastructure just to name a few— revealed several things.
One, there is no uniform standard to measure to quality of health care and performance in hospitals.
"Standardization of care not a common practice in LGU and private hospitals. Both public and private hospitals do not use relevant quality and efficiency indicators in measuring their performance. Significant number of hospitals do not practice systemic target management," Ulep- who is one of the authors of the study, said in his conclusion.
Some hospitals even "lack basic diagnostic equipment".
"20 percent of all hospitals have no electronic medical record… few hospitals do not have X- ray, ECG, and ultrasound equipment present, while all facilities have laboratories, a few (8 percent) hospitals do not meet standards for their facility level or have functional sterilization equipment around 18 percent," Ulep said.
Electricity, water, waste disposal and ambulances continue to be a challenge in some hospitals.
"While all hospitals have electricity, only 31 percent have reliable generator. If you look at the WHO, it is one measure of resilience, that all hospitals should have functional generators. 30 percent have no access to clean drinking water…for water disposal, 24 percent have access to landfill, for ambulances 86 percent have at least 1 emergency vehicle and meet DOH standards," Ulep said.
There are also a number of hospitals who do not meet required staffing standards, with a high turnover particularly for nurses, particularly in private hospital at 22.5%.
Essential medicines required by the WHO are not available in some hospitals.
"Only 3 percent of LGU hospitals surveyed have the complete essential drugs. 55 percent for public national hospitals and 20 percent in private hospitals. In other words, kokonti lang ang nagke-carry ng complete drugs," Ulep said.
To improve, the senior research fellow recommended a couple of things: One, is to "systematically collect and measure a wide range of quality health indicators".
"The Department of Health should lead the development of comprehensive health information standards- I want to highlight the word ‘standard’ to that we will be able to capture comprehensive elements of health care quality, not only structure based but interaction, process and outcomes," Ulep said.
And two, "hinge quality of healthcare to financing".
"Leveraging Philhealth and its ability to provide grants for them for hospital to submit healthcare quality data, and to design provider payments to leverage quality, like provisions of incentives and disincentives," Ulep said.
"I know this is far discussions yet I think it is important for us to move in that direction as many mature health systems are doing. leveraging quality of care using financing tools, and less of regulatory compliance," he added.
SECOND STUDY
Titled "An Assessment of the Quality of Inpatient Meals and Nutrition and Dietetics Processes in Select Public Hospitals in the Philippines", the researchers conducted online surveys on all 428 DOH and LGU-owned public hospitals.
It revealed that lack of resources is preventing hospitals to achieve "its objective of providing quality care".
For one, they are "unable to meet minimum meal allowance per capita and the required nutritional content of planned meals".
More resources are needed to boost human resources, as well as achieve food service process standards among others.
"The most unequipped hospitals were LGU- owned hospitals, specifically LGU Level 1 hospitals which may reflect socioeconomic inequity in the provision of quality nutrition care," Lyle Daryll Casas, Research Analyst of PIDS said.
According to DOH Administrative Order 2016- 0020, at least P150 minimum meal allowance is allotted for each patient per day, providing least 1,800 calories.
"Quality nutrition care in hospitals is critical as this is when patients are in most need of good nutrition for their recovery. Poor dietary intake that results in malnutrition can lead to longer recovery time, higher risks in complications, or worsening of patient’s health during admission," Casas said.
But the problem is, public hospitals can’t even achieve this.
The reason? The study concluded "Limited budget and high costs in the area and 80 percent of hospitals perceive P150 as insufficient".
"The prescribed 1,800 calories… is not being met by half of the hospitals. In terms of macronutrient content, all hospitals did not meet the acceptable distribution range for carbohydrates, proteins and fats. Nevertheless, there is a high compliance of protein requirement at 78.2 percent while the lowest compliance was carbohydrates at 29.3 percent. this pattern was similar across the different levels of government hospitals," Casas said.
Meanwhile, only 33 percent of hospitals have weighing scale and stadiometer.
Some hospitals do not even have standardized recipes for their patients.
Most hospitals skip “food weighing of cooked meals”.
"Inconsistent meal portions may lead to emergency purchase of additional ingredients outside the projected quantities which can contribute to the higher prices of food items," Casas added.
Hence, PIDS recommended a "review" on the policy on standardized meal allowance, capacitate registered nutritionists and dietitians to achieve “better and more efficient meal planning and procurement practices”, provide learning and development interventions, and update the new staffing pattern.
DOH REACTION
The Department of Health "recognizes" the "large gap" in the implementations of standards revealed in the studies.
"There are a lot of programs under the Department of Health that really measures quality, but what’s more important is to see these indicators in a more systematic manner," DOH OIC- Division Chief of Policy, Planning, and Program Division, Health Facility Development Bureau Dr. Terence Antonio said.
What the DOH plans to do now is to "revisit" the overall direction and strengthen the Integrated Hospital Operations Management Program or IHOME, which has been existing for years.
The program "ensures the implementation of standards and guidelines" to "improve efficiency and effectiveness of health care services".
"The particular shift is in the overall direction which intends to expand the program in terms of scope, those being used and innovating program delivery. We also recognize, with the overall devolution transition plan, we really need to capacitate our Local government units in terms of how they will manage health facilities," Antonio said.
Some of their strategies include implementing "innovative platforms", "converting manuals to e-books", "harmonizing data collection", and "expansion of scope with other hospital systems to adopt DOH standards".
DOH vowed that they will look into the deficiencies mentioned in the studies.
"The study has identified the strength and weaknesses in the system in terms of nutrition and dietetics," DOH Health Facility Development Bureau Dietary Adviser Josephine Guiao said.
One of the developments they are working on is the issuance of a new administrative order or AO.
"An updated per capita meal allowance for inpatients has now been ratified and awaiting the signature of the DOH secretary. There will be training on the nutritional care process for private and public hospitals to cater for the critically ill...this coming 3rd and 4th quarter of 2022," Guiao added.
WHAT TO RECOMMEND TO MARCOS ADMINISTRATION
PIDS believes that the incoming administration can use incentives to push for changes to beef up qualify health care in hospitals.
"Link quality to incentives. Many countries have done it. It is not all about compliance regulation. The power of incentives and intent...could be the possible driver of higher quality of care practice," Ulep said.
Monitoring and evaluation of hospital care is also necessary.
"It is important to start examining especially ng private hospital… the variation of quality is massive. We need better monitoring and evaluation both for public, especially for private hospitals," Ulep said.
But at the end of the day, Ulep believes that the Marcos administration should simply implement the law.
"This is already anchored in the UHC (Universal Health Care), basically kailangan lang gawin ng next admin is to implement the UHC law," Ulep said.