THE foot-thick walls of Catanduanes province’s biggest health facility have withstood winds howling from the east. Then Covid-19 Patient No. 25 walked inside, and the echoes of her cough made the walls seemingly tremble.
Protocols were followed, according to Eastern Bicol Medical Center (EBMC) Hospital Chief Dr. Vietrez D. Abella. Using outdated machines, they confirmed the 63-year-old female patient’s fever and complaints of sore throat are symptoms of the coronavirus disease 2019 (Covid-19) infection. Patient 25 also admitted to having returned from a trip to Japan.
However, the two-storey EMBC didn’t have an isolation room. The hospital scrambled to build one but acquiring construction materials proved to be another uphill battle.
Lumber supply was out of stock from the very few hardware stores that still opened under Luzon island’s enhanced community quarantine (ECQ). Luckily, the province’s environment officer donated 80 pieces of 2x2x12 wood.
An online appeal was made: the Level-II apex hospital needed facemasks, alcohol and personal protective equipment (PPE) sets for its health workers, Maria Angela Valeza posted on Facebook. Generosity from provincemates poured and kept pouring in for the EMBC, located in Catanduanes capital Virac.
Abella said all the staff was ordered to go on 14-day quarantine.
However, those outside of EMBC’s aegis didn’t, as health workers in Catanduanes soldiered on to confront an unseen enemy that quietly invaded a serene island-paradise called “The Land of the Howling Winds.”
Indeed, Patient 25’s medical condition not only rattled the state of affairs at EBMC: it also showed the shaky foundations of a public hospital and the country’s health system.
Resource generation
THE 100-bed Center had to be innovative given the pandemic. Abella said temporary triage and holding areas were set up for suspected patients.
Rooms in the pay ward (including an operating room and a delivery room) became temporary isolation rooms. It is in these temporary rooms where the 80 pieces of lumber were used.
EMBC then started “gate-keeping” by prioritizing cases “appropriate to its level of care as a general hospital with medical specialists,” Abella tells this newspaper. Those with mild respiratory infections, gastroenteritis and simple urinary tract infections were referred to Level 1 and district hospitals in Virac, Pandan, San Andres, Caramoran, Viga and Gigmoto (one per municipality, for a total of six).
On May 3, the Department of Science and Technology (DOST) handed to EMBC one of six Covid-19 specimen booths for the entire Bicol region. This white-paneled booth, with glass encasing and two rubberized black gloves, now greets visitors at the EMBC.
In some ways, EMBC is holding on; not so the provincial government.
Last May 11, the provincial legislative council unanimously approved a resolution reverting the EMBC back to the Department of Health (DOH) as a provincial hospital.
Economic enterprise
SINCE the capitol released Ordinance 2010-001 declaring the EMBC a local government-run economic enterprise, the Center has been suffering “heavy economic losses” the last few years, according to Provincial Board Member Santos V. Zafe.
Speaking in a personal capacity, Abella confirmed that the hospital “had serious cash flow issues” that led to delayed salaries from 2013 to 2016.
Not surprisingly, some island residents have complained of poor services from EMBC. While it is easy to refer cases to other hospitals in the province or in mainland Luzon, situations of lockdown and referral for Catanduganons with severe cases would require them to take a three-hour to four-hour ride via ferry.
And if EMBC would like to be a fully-functioning hospital that complies with DOH standards, the average resources it needs from now until 2024 is P229 million —a fifth of the province’s annual budget.
Fighting Covid-19
THE Philippines’ army of public hospitals and local government-owned rural health units (RHUs) and barangay health centers (BHCs) are on their toes fighting the pandemic. Privately-run health facilities, the ones with reputedly better medical care, have also joined the fray.
But even if these 1,224 hospitals, 2,581 RHUs and 20,216 BHCs —in locked lands and in island communities, both densely and sparsely populated— band together, they are all burdened.
The weight of this burden is systemically seen: unequal access to better care; decrepit public health facilities; fragmented, uncoordinated health management across geographies; and, under-resourced health programs. There’s also largely household-driven health spending that drives away the poor and drains moneyed folk and the unwieldy regulation of health interventions.
Assessments past and present by Filipino health policy experts and practitioners about the systemic issues of the Philippine health system are like Catanduanes’ howling winds during typhoons: they still shriek.
Ongoing battle
INDEED, the pandemic exposed the sordid state of the country’s health system, which former health secretary Manuel M. Dayrit described as “not modernized.”
“Our system is not ready (for the pandemic),” this former director of the World Health Organization (WHO) told a virtual hearing by the House of Representatives mid-April. “We have to admit that [that] is the description of [our] health system.”
Such frank assessment lurks as countries’ health officials—during the recent virtual World Health Assembly last May 18 to May 19—said they continue to find ways to fight SARS-CoV-2 with what they have and with the way their health systems are run.
These economies’ ongoing battle against Covid-19 also comes at the heels of the Philippines’ first full-year foray into universal health care after the signing of Republic Act 11223 in February last year.
Real costs
THE cost of two short jeepney rides per day is all it took for every Filipino to pay for their daily health needs in 2018. But the truth is, this cost is too high a price, being on top of their food and non-food needs.
Based on the latest Philippine National Health Accounts (PNHA) data, the Philippine Statistics Authority (PSA) estimated that individual Filipinos’ health in 2018 grew by 6.6 percent to P7,496. In real terms, and using 2018 as base year, per capita health expenditure of Filipinos amounted to P6,391.
But even under a new base year to compute expenditures made by the economy, this trend persists: households still accounted for the bulk of health expenses made. Of the P766.86-billion health spending made in 2018, more than half (58.6 percent) or P449.17 billion was spent by households through out-of-pocket (OOP) payments.
The national government only spent 29.8 percent (P228.86 billion) of the total, while corporations spent 2.6 percent or P20.11 billion in 2018.
Using old-base years to compute total health expenditures, comparable PNHA data from 1994 to 2014 (excluding unavailable 2006 data) showed OOP payments from households make up an average of 50.41 percent of total health expenditures.
Average national government spending for health is 15.98 percent; it’s 14.78 percent for local governments; and, is 7.97 percent from the Philippine Health Insurance Corp. (PhilHealth).
Measure reformed
PAYMENTS for health care were previously made through fee-for-payment schemes.
This measure was reformed in 2013 through PhilHealth’s mandating of case rates. But Dayrit and three other health experts wrote in a 2018 assessment of the country’s health system that such case rates approach “has not resulted [in] technical efficiency, much less financial protection.”
“Health facilities can set their own service charges and then bill the patient whatever share of the service charge that isn’t covered by the PhilHealth case rate,” wrote Dayrit, Liezel P. Lagrada, Oscar F. Picazo, Melahi C. Pons and Mario C. Villaverde in the WHO-funded 2018 Philippine Health System Review.
Most of the OOP payments are for medicines, what with pre-RA 11223 benefits of PhilHealth not covering a comprehensive outpatient primary care benefit, Dr. Ramon Pedro Paterno of the University of the Philippines explained.
“A failure in spending enough at the lower levels of health care leads to higher spending at the higher levels,” said Paterno, a research faculty for UP’s Institute of Health Policy and Development Studies.
High fixed ceiling
ON one hand, rising OOP spending may mean Filipinos are trying to pay for better but more expensive medical care, according to a 2017 report by the UPecon Foundation of the UP School of Economics.
On the other hand, because a PhilHealth benefit has a high fixed ceiling, the support value of such benefit “declines as total health care bills increase.”
“This pressure increases as both public and private (health) facilities respond to rising demand,” physicians Carlo Irwin A. Panelo and Rebecca Q. Ramos and economists Orville C. Solon and Alejandro N. Herrin wrote in the report.
Historically-rising OOP shares to total health expenditures is not only a households’ response to the fee-for-service system. Panelo and colleagues wrote the health system “misses out on the efficiency gains of risk pooling,” or sharing the burden of health costs.
“Individual families will have to set aside resources equivalent to the average cost of hospitalization in the face of health risks,” the authors of “The Challenge of Reaching the Poor with a Continuum of Care: A 25-Year Assessment of the Philippine Health Sector” said.
Unsurprisingly, targeting health services for the poor is not done effectively while support for their health needs coming from public funds also inadequate. Panelo and colleagues wrote: “Moreover, when budgets are lacking, public facilities will increasingly rely on ‘outside purchases.’”
Entire sector
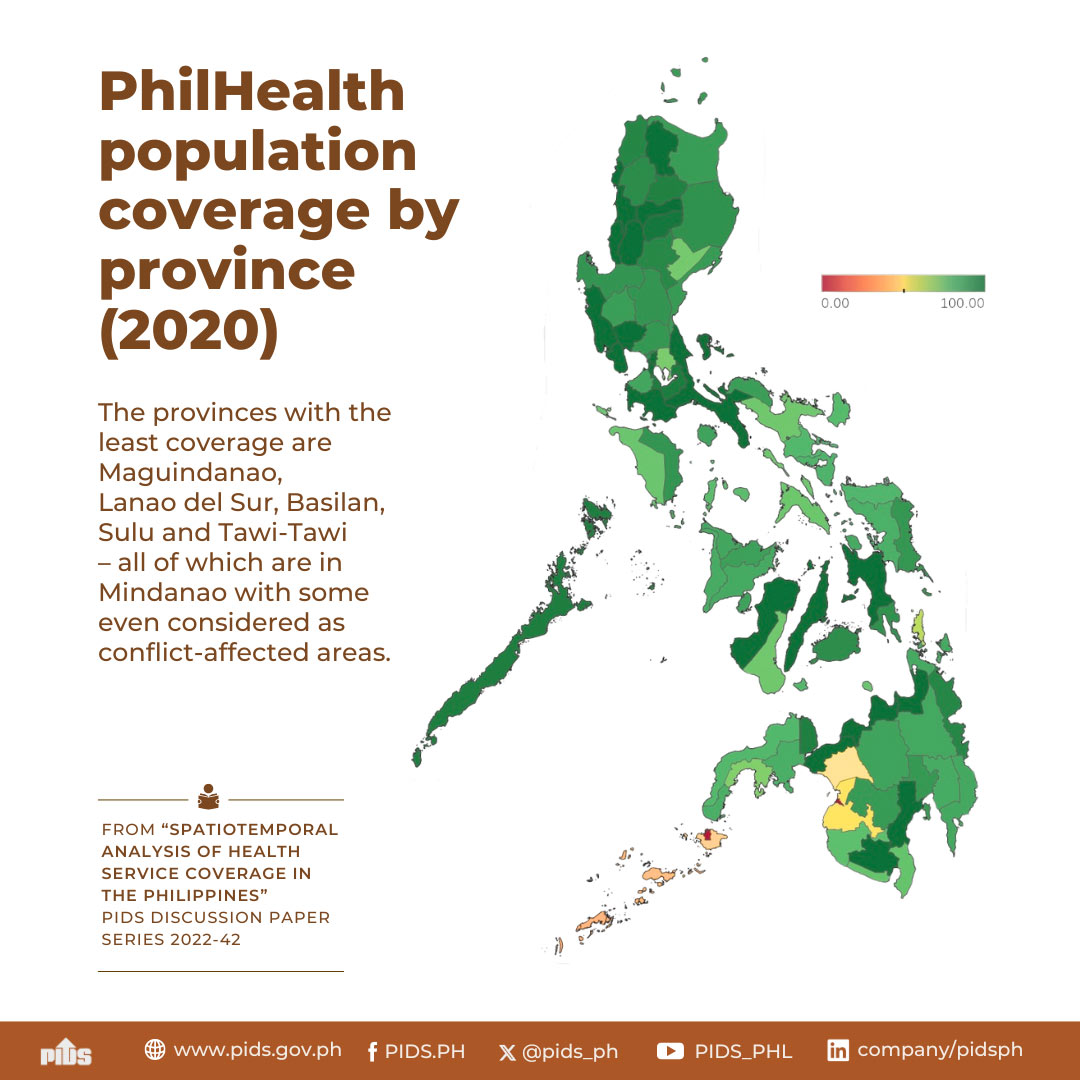
PHILHEALTH Vice President for Corporate Affairs Shirley B. Domingo told a May 15 webinar by the Filipino-run group Rights Corridor the new UHC law now provides inpatient and outpatient benefits to all Filipinos. All Filipinos are now mandatory members of PhilHealth, the country’s social-health insurer.
As for payments, Domingo says the new UHC will lead to better risk pooling of health expenses given the prospective implementation of PhilHealth’s “fixed payment rate.” In this new approach, patients and their families will now know how much to shell out.
However, Domingo tells webinar participants that Filipino workers at home and abroad are required to pay premiums. These premiums have increments annually, from this year up to 2024, which can reach up to five percent of one’s monthly salary.
Local workers (classified by PhilHealth as “direct contributors”) and their employers pay equal share to a worker’s PhilHealth premiums through automatic salary deductions.
Meanwhile, those called “indirect contributors” of PhilHealth membership, such as workers in the informal economy and overseas Filipinos, will bear the full costs of monthly premiums.
Apart from the PhilHealth premium payments, national and local tiers of government subsidize health care for senior citizens, indigents and people with disabilities (PWDs). Health funds also get allocations from the Philippine Charity Sweepstakes Office (40 percent of PCSO’s charity fund) and the Philippine Amusement and Gaming Corp. (50 percent of Pagcor’s share). Republic Act 10351 or the sin tax law had also provided earnings for health.
All these revenue sources are “attributed to the entire health sector,” Undersecretary Tina Rose Marie L. Canda of the Department of Budget and Management told the BusinessMirror.
A small base
TO implement the gradual reforms of the UHC law, Health Secretary Francisco T. Duque III and Finance Secretary Carlos G. Dominguez said the country needs P1.44 trillion. Earmarked thus far is P1.01 trillion. That is why both officials asked Congress a year ago that excise tax rates for tobacco and liquor be raised to cover the financing gap of P426 billion.
Nevertheless, government appropriations and taxes —not PhilHealth premiums— must be the main source of funds for UHC so as to slash high OOP share to total health expenditures, Paterno said
Citing a WHO study on global health financing, Paterno said low- and middle-income countries like the Philippines must have government appropriations as “the main source of compulsory revenues for the health system.” This is because the country has a visible number of informal workers and poor families.
PhilHealth premiums will not be enough to finance UHC, Paterno said, “given the structure of the economy and a small levy base.”
“Innovative health financing” schemes such as sin taxes are also not enough, Paterno said adding that OOP payments are also “a regressive way to fund health services.”
Localized system
BUT even as efforts to reform health financing are being done, a bigger elephant in the room is the archipelago with thousands of localized health systems.
The 1991 Local Government Code (Republic Act 7160) had devolved many health services to LGUs. This led to the creation of provincial, city and health offices while expanding the number of RHUs and BHCs to tailor health interventions to local health needs.
Since 1992, DOH has been providing nationwide policy direction, health standards and guidelines as well as highly-specialized, specific tertiary health services through the tertiary hospitals the agency manages.
Some experts blame the devolution of health service delivery for failing to address the needs of the poor, and even for fragmented health interventions and financing.
Turning back
PANELO and colleagues (in the UPecon Foundation of the UP School of Economics report) wrote that since LGUs are less-capable handling of health needs, they had fragmented the “previously integrated network of public health facilities, personnel and budget.”
Health devolution had all but weakened the ability of local health care systems to deliver health services, especially to the poorest, they added.
De La Salle University economist Maria Ella C. Oplas agrees: resource issues encountered by hospitals like EBMC are mainly rooted in this fragmented health system.
Many LGUs are ill-equipped to search for health funds, are short of manpower, and even have networks to access private sector funds “which could come in handy in dire straits,” Oplas said.
That’s why “some hospitals actually want to go back under DOH jurisdiction again,” she added.
Dayrit and his colleagues also said that devolution “increased health service coverage, including facility-based deliveries and utilization of inpatient and outpatient care.”
Health access
HOWEVER, Michael Ralph M. Abrigo of the Philippine Institute of Development Studies (PIDS) said devolution is not the “root cause” why the Philippine health system is egregious.
Abrigo said increased health access have led “to positive impacts on health outcomes, when we consider (findings from) better-designed research.”
Even decentralization and some increases in LGUs’ annual budgets for health “did not result to better health-seeking behaviors,” Abrigo said citing a PIDS study on pregnant women.
The greater amount of LGUs for health “does not readily translate to greater health expenditures as local governments may have other [development] priorities,” Abrigo told the BusinessMirror.
Local hospitals like EMBC are left to find means to become economically viable.
According to Abella, around 70 percent of EBMC’s annual income comes from reimbursement of PhilHealth claims. The rest comes from non-cash assistance from a DOH program for health facilities and from the PCSO.
Suffering cuts
ACCORDING to University of Santo Tomas Medical Professor Dr. Maria Minerva P. Calimag, politics also contributed to the problems surrounding health devolution.
While the DOH budget posted a 2.98-percent growth to P100.56 billion under the 2020 General Appropriations Act (GAA) from P97.65 billion in 2019, there were budget cuts for health facilities. The area that suffered the largest budget cut was the Epidemiology and Surveillance Program (ESP). The budget for ESP in 2020 was slashed by 56.08 percent to P115.51 million from P262.997 million.
Locally, Abrigo adds, generally low resources of LGUs are reflected in not just health funds but also in other basic services locally.
“Our presumption, when we devolved health, was that there is integrity within the system: there’s no conflict of interest [and] there’s transparency, accountability and good governance,” said Calimag, a former president of the Philippine Medical Association.
She said health should be the priority of the government and the highest budget should be allocated to it.
“At the end of the day, if your people are sickly, apart from spending higher amounts for further care, you have lost manpower on other things that needed to be done,” Calimag said.
Yawning issue
WHAT health devolution may have also contributed is the problematic coordination between and among public and private health care providers for Filipinos’ primary health care needs—from initial diagnosis to recovery and palliative care.
Since 1992, the health system had become “pluralistic” in service delivery, Dayrit and colleagues wrote.
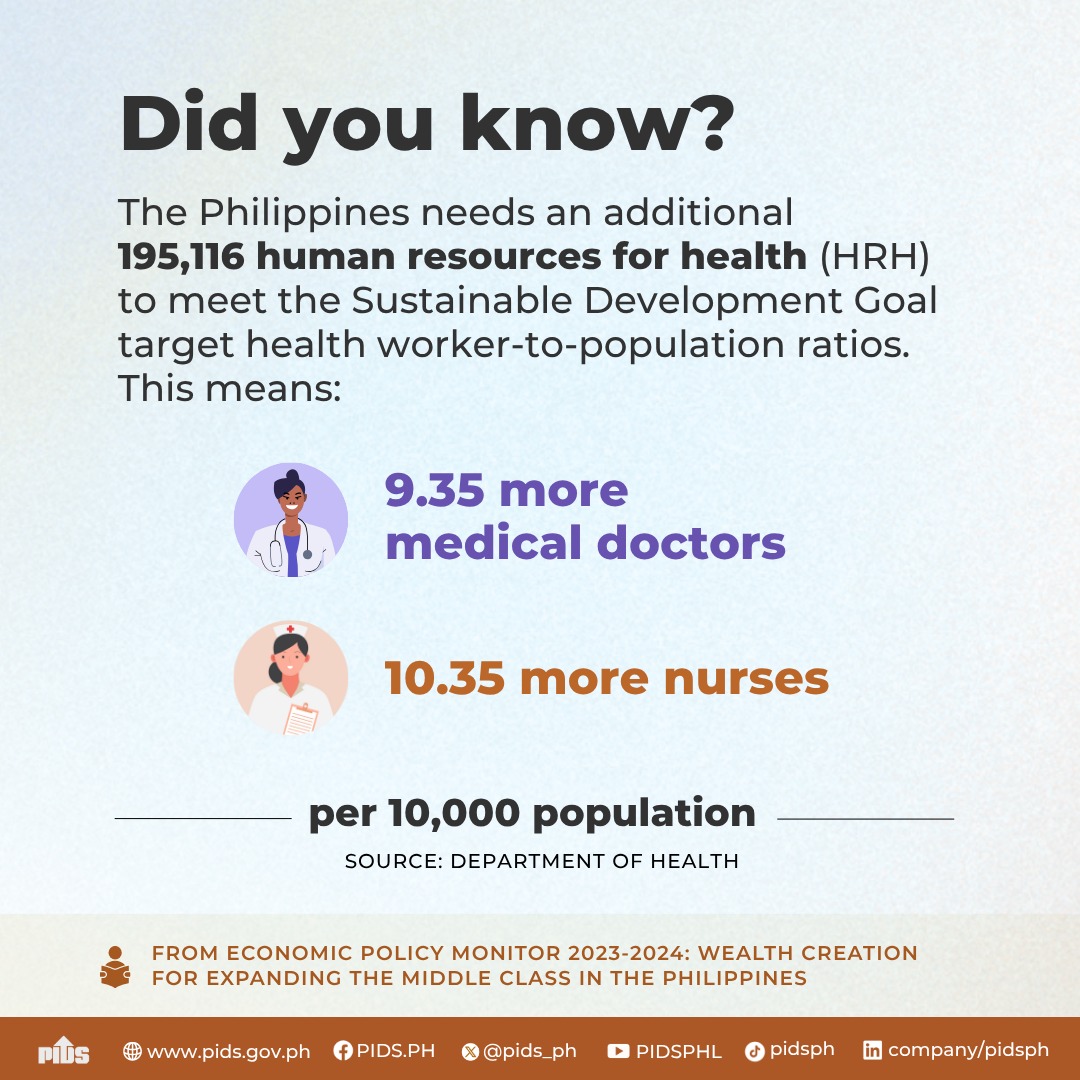
As well, the more endowed Philippine regions have the better health care facilities and equipment. Meanwhile, given the presence of 90,308 nurses, 40,775 doctors, 43,044 midwives, and 13,413 medical technologists nationwide, these health workers are abundant in developed regions and sparse in poorer Philippine regions, Panelo’s report wrote.
Thus, this “pluralistic” health system led to variations in health service delivery, with lagging regions behind in providing quality care, Panelo wrote.
Geographic factors also hinder delivering quality care, like the remoteness of mountainous regions and remote islands, according to Abrigo. Calimag added that high security risks prompt health workers to also avoid these areas.
Slipped goals
THE “devolved” health system may have inadvertently led to citizens’ disturbing health conditions.
Panelo and colleagues bared in their report that health targets for maternal, infant and child mortality, child under-nutrition and tuberculosis under the old Millennium Development Goals were not met.
Devolution also negatively affected the ability of local health systems to respond to emerging and re-emerging infectious diseases (Ereids), like Covid-19.
Even before Covid-19, Panelo and colleagues had doubted the ability of the country to respond effectively to challenges from disease outbreaks. Their 2017 assessment even called on government to “build capacities to respond to Ereids” as overseas Filipinos and tourists will be the next pathogen carriers.
And the poor will be more vulnerable from community-level disease transmission “owing to weaker health status, lack of knowledge of the disease, poor health-seeking behavior and limited access to health services, including that for surveillance and containment of emerging diseases,” Panelo and colleagues wrote.
Targeted risks
GIVEN these realities, Domingo said the UHC law will see DOH implementing a functional “Service Delivery Network,” or SDN. This platform is expected to integrate the network of fragmented health care providers in an area’s health system.
The SDN will integrate private and publicly-run health facilities, diagnostic centers, laboratories pharmacies into a “primary care provider network” so that referred patients’ needs are facilitated and addressed even when they’re recuperating in home communities, Domingo said.
The SDN will also be operationalizing an approach called “Konsultasyong Sapat at Tama,” or Konsulta (consult), covering both private and public health facilities. Covered in Konsulta are initial and follow-up consultations, targeted health risk screening and assessment, some diagnostic tests and some medicines, Domingo explained during the May 15 webinar.
She added these reform measures under the UHC law will be gradually implemented from 2020 up to 2024, coinciding with the new premium rates for PhilHealth.
Per-year changes include the following: expanding primary care benefits (2021); expanding such benefits to include emergency services and outpatient drugs (2022); integrating the SDN (2023); and, increasing the support value for inpatient care and for addressing debilitating diseases, and integrating health care financing and patient referral (2024 onwards).
“UHC is a very nice (health) reform measure,” Domingo told webinar participants, “that addresses risk pooling (of expenses) and builds social solidarity for the health needs of those who can’t afford.”
Eye-opener
THE Panelo assessment report of 2017 and the Dayrit report of 2018 had many wish lists for the country’s health system.
Common recommendations include consolidating national and local health care financing; strengthening the capacities of health facilities and their workers under a localized, fragmented health system set-up; and, implementing the SDN.
Meanwhile, recent international assessments on national health systems’ response to infectious diseases are giving eye-openers to Filipino health authorities.
Last February, The Nuclear Threat Initiative and the Johns Hopkins University’s Bloomberg School of Public Health released results of the 2019 Global Health Security Index to assess countries’ readiness to biological threats and infectious diseases. The Philippines ranked 53rd out of 195 countries with an index score of 47.6.
That Index had six indicators: prevention from pathogens; detection and reporting of epidemics; rapid response and mitigation of epidemics; risk environment and vulnerability to biological threats; compliance with international norms on health capacity and financing; and sufficient and robust health system. The Philippines scored the lowest in the “health system” (sub-indicator score: 38.2) and “prevention” (38.5) indicators.
A major player in the fight against the pandemic is the Research Institute for Tropical Medicine (RITM). This DOH unit got P519 million in this year’s budget, spearheading the nation’s Covid-19 testing efforts.
Making do
FOR now, the Philippines contends with nearly-13,000 Covid-19 cases, including deaths and recoveries. Over 1,500 health workers have contracted the deadly virus. More than 30,000 overseas Filipino workers, displaced from their host countries and from their ships, have been repatriated.
The hospitals and health facilities in the richer provinces, cities and municipalities not only have more Covid-19 cases; they’re heavily burdened. Contrast this to the burden of developed regions and 42 provinces, like Catanduanes, with no or limited Covid-19 cases.
In the meantime, health facilities in provinces like Catanduanes would have to make do with the support of politicians and private donors.
And the May 11 resolution of the province’s legislative council, a funding window was shut.
Indeed, the country’s health system must rely not on cash but the compassion and profession of professional health workers.
They form the only abundant resource this country has to be strong against the howling winds of Covid-19.
Protocols were followed, according to Eastern Bicol Medical Center (EBMC) Hospital Chief Dr. Vietrez D. Abella. Using outdated machines, they confirmed the 63-year-old female patient’s fever and complaints of sore throat are symptoms of the coronavirus disease 2019 (Covid-19) infection. Patient 25 also admitted to having returned from a trip to Japan.
However, the two-storey EMBC didn’t have an isolation room. The hospital scrambled to build one but acquiring construction materials proved to be another uphill battle.
Lumber supply was out of stock from the very few hardware stores that still opened under Luzon island’s enhanced community quarantine (ECQ). Luckily, the province’s environment officer donated 80 pieces of 2x2x12 wood.
An online appeal was made: the Level-II apex hospital needed facemasks, alcohol and personal protective equipment (PPE) sets for its health workers, Maria Angela Valeza posted on Facebook. Generosity from provincemates poured and kept pouring in for the EMBC, located in Catanduanes capital Virac.
Abella said all the staff was ordered to go on 14-day quarantine.
However, those outside of EMBC’s aegis didn’t, as health workers in Catanduanes soldiered on to confront an unseen enemy that quietly invaded a serene island-paradise called “The Land of the Howling Winds.”
Indeed, Patient 25’s medical condition not only rattled the state of affairs at EBMC: it also showed the shaky foundations of a public hospital and the country’s health system.
Resource generation
THE 100-bed Center had to be innovative given the pandemic. Abella said temporary triage and holding areas were set up for suspected patients.
Rooms in the pay ward (including an operating room and a delivery room) became temporary isolation rooms. It is in these temporary rooms where the 80 pieces of lumber were used.
EMBC then started “gate-keeping” by prioritizing cases “appropriate to its level of care as a general hospital with medical specialists,” Abella tells this newspaper. Those with mild respiratory infections, gastroenteritis and simple urinary tract infections were referred to Level 1 and district hospitals in Virac, Pandan, San Andres, Caramoran, Viga and Gigmoto (one per municipality, for a total of six).
On May 3, the Department of Science and Technology (DOST) handed to EMBC one of six Covid-19 specimen booths for the entire Bicol region. This white-paneled booth, with glass encasing and two rubberized black gloves, now greets visitors at the EMBC.
In some ways, EMBC is holding on; not so the provincial government.
Last May 11, the provincial legislative council unanimously approved a resolution reverting the EMBC back to the Department of Health (DOH) as a provincial hospital.
Economic enterprise
SINCE the capitol released Ordinance 2010-001 declaring the EMBC a local government-run economic enterprise, the Center has been suffering “heavy economic losses” the last few years, according to Provincial Board Member Santos V. Zafe.
Speaking in a personal capacity, Abella confirmed that the hospital “had serious cash flow issues” that led to delayed salaries from 2013 to 2016.
Not surprisingly, some island residents have complained of poor services from EMBC. While it is easy to refer cases to other hospitals in the province or in mainland Luzon, situations of lockdown and referral for Catanduganons with severe cases would require them to take a three-hour to four-hour ride via ferry.
And if EMBC would like to be a fully-functioning hospital that complies with DOH standards, the average resources it needs from now until 2024 is P229 million —a fifth of the province’s annual budget.
Fighting Covid-19
THE Philippines’ army of public hospitals and local government-owned rural health units (RHUs) and barangay health centers (BHCs) are on their toes fighting the pandemic. Privately-run health facilities, the ones with reputedly better medical care, have also joined the fray.
But even if these 1,224 hospitals, 2,581 RHUs and 20,216 BHCs —in locked lands and in island communities, both densely and sparsely populated— band together, they are all burdened.
The weight of this burden is systemically seen: unequal access to better care; decrepit public health facilities; fragmented, uncoordinated health management across geographies; and, under-resourced health programs. There’s also largely household-driven health spending that drives away the poor and drains moneyed folk and the unwieldy regulation of health interventions.
Assessments past and present by Filipino health policy experts and practitioners about the systemic issues of the Philippine health system are like Catanduanes’ howling winds during typhoons: they still shriek.
Ongoing battle
INDEED, the pandemic exposed the sordid state of the country’s health system, which former health secretary Manuel M. Dayrit described as “not modernized.”
“Our system is not ready (for the pandemic),” this former director of the World Health Organization (WHO) told a virtual hearing by the House of Representatives mid-April. “We have to admit that [that] is the description of [our] health system.”
Such frank assessment lurks as countries’ health officials—during the recent virtual World Health Assembly last May 18 to May 19—said they continue to find ways to fight SARS-CoV-2 with what they have and with the way their health systems are run.
These economies’ ongoing battle against Covid-19 also comes at the heels of the Philippines’ first full-year foray into universal health care after the signing of Republic Act 11223 in February last year.
Real costs
THE cost of two short jeepney rides per day is all it took for every Filipino to pay for their daily health needs in 2018. But the truth is, this cost is too high a price, being on top of their food and non-food needs.
Based on the latest Philippine National Health Accounts (PNHA) data, the Philippine Statistics Authority (PSA) estimated that individual Filipinos’ health in 2018 grew by 6.6 percent to P7,496. In real terms, and using 2018 as base year, per capita health expenditure of Filipinos amounted to P6,391.
But even under a new base year to compute expenditures made by the economy, this trend persists: households still accounted for the bulk of health expenses made. Of the P766.86-billion health spending made in 2018, more than half (58.6 percent) or P449.17 billion was spent by households through out-of-pocket (OOP) payments.
The national government only spent 29.8 percent (P228.86 billion) of the total, while corporations spent 2.6 percent or P20.11 billion in 2018.
Using old-base years to compute total health expenditures, comparable PNHA data from 1994 to 2014 (excluding unavailable 2006 data) showed OOP payments from households make up an average of 50.41 percent of total health expenditures.
Average national government spending for health is 15.98 percent; it’s 14.78 percent for local governments; and, is 7.97 percent from the Philippine Health Insurance Corp. (PhilHealth).
Measure reformed
PAYMENTS for health care were previously made through fee-for-payment schemes.
This measure was reformed in 2013 through PhilHealth’s mandating of case rates. But Dayrit and three other health experts wrote in a 2018 assessment of the country’s health system that such case rates approach “has not resulted [in] technical efficiency, much less financial protection.”
“Health facilities can set their own service charges and then bill the patient whatever share of the service charge that isn’t covered by the PhilHealth case rate,” wrote Dayrit, Liezel P. Lagrada, Oscar F. Picazo, Melahi C. Pons and Mario C. Villaverde in the WHO-funded 2018 Philippine Health System Review.
Most of the OOP payments are for medicines, what with pre-RA 11223 benefits of PhilHealth not covering a comprehensive outpatient primary care benefit, Dr. Ramon Pedro Paterno of the University of the Philippines explained.
“A failure in spending enough at the lower levels of health care leads to higher spending at the higher levels,” said Paterno, a research faculty for UP’s Institute of Health Policy and Development Studies.
High fixed ceiling
ON one hand, rising OOP spending may mean Filipinos are trying to pay for better but more expensive medical care, according to a 2017 report by the UPecon Foundation of the UP School of Economics.
On the other hand, because a PhilHealth benefit has a high fixed ceiling, the support value of such benefit “declines as total health care bills increase.”
“This pressure increases as both public and private (health) facilities respond to rising demand,” physicians Carlo Irwin A. Panelo and Rebecca Q. Ramos and economists Orville C. Solon and Alejandro N. Herrin wrote in the report.
Historically-rising OOP shares to total health expenditures is not only a households’ response to the fee-for-service system. Panelo and colleagues wrote the health system “misses out on the efficiency gains of risk pooling,” or sharing the burden of health costs.
“Individual families will have to set aside resources equivalent to the average cost of hospitalization in the face of health risks,” the authors of “The Challenge of Reaching the Poor with a Continuum of Care: A 25-Year Assessment of the Philippine Health Sector” said.
Unsurprisingly, targeting health services for the poor is not done effectively while support for their health needs coming from public funds also inadequate. Panelo and colleagues wrote: “Moreover, when budgets are lacking, public facilities will increasingly rely on ‘outside purchases.’”
Entire sector
PHILHEALTH Vice President for Corporate Affairs Shirley B. Domingo told a May 15 webinar by the Filipino-run group Rights Corridor the new UHC law now provides inpatient and outpatient benefits to all Filipinos. All Filipinos are now mandatory members of PhilHealth, the country’s social-health insurer.
As for payments, Domingo says the new UHC will lead to better risk pooling of health expenses given the prospective implementation of PhilHealth’s “fixed payment rate.” In this new approach, patients and their families will now know how much to shell out.
However, Domingo tells webinar participants that Filipino workers at home and abroad are required to pay premiums. These premiums have increments annually, from this year up to 2024, which can reach up to five percent of one’s monthly salary.
Local workers (classified by PhilHealth as “direct contributors”) and their employers pay equal share to a worker’s PhilHealth premiums through automatic salary deductions.
Meanwhile, those called “indirect contributors” of PhilHealth membership, such as workers in the informal economy and overseas Filipinos, will bear the full costs of monthly premiums.
Apart from the PhilHealth premium payments, national and local tiers of government subsidize health care for senior citizens, indigents and people with disabilities (PWDs). Health funds also get allocations from the Philippine Charity Sweepstakes Office (40 percent of PCSO’s charity fund) and the Philippine Amusement and Gaming Corp. (50 percent of Pagcor’s share). Republic Act 10351 or the sin tax law had also provided earnings for health.
All these revenue sources are “attributed to the entire health sector,” Undersecretary Tina Rose Marie L. Canda of the Department of Budget and Management told the BusinessMirror.
A small base
TO implement the gradual reforms of the UHC law, Health Secretary Francisco T. Duque III and Finance Secretary Carlos G. Dominguez said the country needs P1.44 trillion. Earmarked thus far is P1.01 trillion. That is why both officials asked Congress a year ago that excise tax rates for tobacco and liquor be raised to cover the financing gap of P426 billion.
Nevertheless, government appropriations and taxes —not PhilHealth premiums— must be the main source of funds for UHC so as to slash high OOP share to total health expenditures, Paterno said
Citing a WHO study on global health financing, Paterno said low- and middle-income countries like the Philippines must have government appropriations as “the main source of compulsory revenues for the health system.” This is because the country has a visible number of informal workers and poor families.
PhilHealth premiums will not be enough to finance UHC, Paterno said, “given the structure of the economy and a small levy base.”
“Innovative health financing” schemes such as sin taxes are also not enough, Paterno said adding that OOP payments are also “a regressive way to fund health services.”
Localized system
BUT even as efforts to reform health financing are being done, a bigger elephant in the room is the archipelago with thousands of localized health systems.
The 1991 Local Government Code (Republic Act 7160) had devolved many health services to LGUs. This led to the creation of provincial, city and health offices while expanding the number of RHUs and BHCs to tailor health interventions to local health needs.
Since 1992, DOH has been providing nationwide policy direction, health standards and guidelines as well as highly-specialized, specific tertiary health services through the tertiary hospitals the agency manages.
Some experts blame the devolution of health service delivery for failing to address the needs of the poor, and even for fragmented health interventions and financing.
Turning back
PANELO and colleagues (in the UPecon Foundation of the UP School of Economics report) wrote that since LGUs are less-capable handling of health needs, they had fragmented the “previously integrated network of public health facilities, personnel and budget.”
Health devolution had all but weakened the ability of local health care systems to deliver health services, especially to the poorest, they added.
De La Salle University economist Maria Ella C. Oplas agrees: resource issues encountered by hospitals like EBMC are mainly rooted in this fragmented health system.
Many LGUs are ill-equipped to search for health funds, are short of manpower, and even have networks to access private sector funds “which could come in handy in dire straits,” Oplas said.
That’s why “some hospitals actually want to go back under DOH jurisdiction again,” she added.
Dayrit and his colleagues also said that devolution “increased health service coverage, including facility-based deliveries and utilization of inpatient and outpatient care.”
Health access
HOWEVER, Michael Ralph M. Abrigo of the Philippine Institute of Development Studies (PIDS) said devolution is not the “root cause” why the Philippine health system is egregious.
Abrigo said increased health access have led “to positive impacts on health outcomes, when we consider (findings from) better-designed research.”
Even decentralization and some increases in LGUs’ annual budgets for health “did not result to better health-seeking behaviors,” Abrigo said citing a PIDS study on pregnant women.
The greater amount of LGUs for health “does not readily translate to greater health expenditures as local governments may have other [development] priorities,” Abrigo told the BusinessMirror.
Local hospitals like EMBC are left to find means to become economically viable.
According to Abella, around 70 percent of EBMC’s annual income comes from reimbursement of PhilHealth claims. The rest comes from non-cash assistance from a DOH program for health facilities and from the PCSO.
Suffering cuts
ACCORDING to University of Santo Tomas Medical Professor Dr. Maria Minerva P. Calimag, politics also contributed to the problems surrounding health devolution.
While the DOH budget posted a 2.98-percent growth to P100.56 billion under the 2020 General Appropriations Act (GAA) from P97.65 billion in 2019, there were budget cuts for health facilities. The area that suffered the largest budget cut was the Epidemiology and Surveillance Program (ESP). The budget for ESP in 2020 was slashed by 56.08 percent to P115.51 million from P262.997 million.
Locally, Abrigo adds, generally low resources of LGUs are reflected in not just health funds but also in other basic services locally.
“Our presumption, when we devolved health, was that there is integrity within the system: there’s no conflict of interest [and] there’s transparency, accountability and good governance,” said Calimag, a former president of the Philippine Medical Association.
She said health should be the priority of the government and the highest budget should be allocated to it.
“At the end of the day, if your people are sickly, apart from spending higher amounts for further care, you have lost manpower on other things that needed to be done,” Calimag said.
Yawning issue
WHAT health devolution may have also contributed is the problematic coordination between and among public and private health care providers for Filipinos’ primary health care needs—from initial diagnosis to recovery and palliative care.
Since 1992, the health system had become “pluralistic” in service delivery, Dayrit and colleagues wrote.
As well, the more endowed Philippine regions have the better health care facilities and equipment. Meanwhile, given the presence of 90,308 nurses, 40,775 doctors, 43,044 midwives, and 13,413 medical technologists nationwide, these health workers are abundant in developed regions and sparse in poorer Philippine regions, Panelo’s report wrote.
Thus, this “pluralistic” health system led to variations in health service delivery, with lagging regions behind in providing quality care, Panelo wrote.
Geographic factors also hinder delivering quality care, like the remoteness of mountainous regions and remote islands, according to Abrigo. Calimag added that high security risks prompt health workers to also avoid these areas.
Slipped goals
THE “devolved” health system may have inadvertently led to citizens’ disturbing health conditions.
Panelo and colleagues bared in their report that health targets for maternal, infant and child mortality, child under-nutrition and tuberculosis under the old Millennium Development Goals were not met.
Devolution also negatively affected the ability of local health systems to respond to emerging and re-emerging infectious diseases (Ereids), like Covid-19.
Even before Covid-19, Panelo and colleagues had doubted the ability of the country to respond effectively to challenges from disease outbreaks. Their 2017 assessment even called on government to “build capacities to respond to Ereids” as overseas Filipinos and tourists will be the next pathogen carriers.
And the poor will be more vulnerable from community-level disease transmission “owing to weaker health status, lack of knowledge of the disease, poor health-seeking behavior and limited access to health services, including that for surveillance and containment of emerging diseases,” Panelo and colleagues wrote.
Targeted risks
GIVEN these realities, Domingo said the UHC law will see DOH implementing a functional “Service Delivery Network,” or SDN. This platform is expected to integrate the network of fragmented health care providers in an area’s health system.
The SDN will integrate private and publicly-run health facilities, diagnostic centers, laboratories pharmacies into a “primary care provider network” so that referred patients’ needs are facilitated and addressed even when they’re recuperating in home communities, Domingo said.
The SDN will also be operationalizing an approach called “Konsultasyong Sapat at Tama,” or Konsulta (consult), covering both private and public health facilities. Covered in Konsulta are initial and follow-up consultations, targeted health risk screening and assessment, some diagnostic tests and some medicines, Domingo explained during the May 15 webinar.
She added these reform measures under the UHC law will be gradually implemented from 2020 up to 2024, coinciding with the new premium rates for PhilHealth.
Per-year changes include the following: expanding primary care benefits (2021); expanding such benefits to include emergency services and outpatient drugs (2022); integrating the SDN (2023); and, increasing the support value for inpatient care and for addressing debilitating diseases, and integrating health care financing and patient referral (2024 onwards).
“UHC is a very nice (health) reform measure,” Domingo told webinar participants, “that addresses risk pooling (of expenses) and builds social solidarity for the health needs of those who can’t afford.”
Eye-opener
THE Panelo assessment report of 2017 and the Dayrit report of 2018 had many wish lists for the country’s health system.
Common recommendations include consolidating national and local health care financing; strengthening the capacities of health facilities and their workers under a localized, fragmented health system set-up; and, implementing the SDN.
Meanwhile, recent international assessments on national health systems’ response to infectious diseases are giving eye-openers to Filipino health authorities.
Last February, The Nuclear Threat Initiative and the Johns Hopkins University’s Bloomberg School of Public Health released results of the 2019 Global Health Security Index to assess countries’ readiness to biological threats and infectious diseases. The Philippines ranked 53rd out of 195 countries with an index score of 47.6.
That Index had six indicators: prevention from pathogens; detection and reporting of epidemics; rapid response and mitigation of epidemics; risk environment and vulnerability to biological threats; compliance with international norms on health capacity and financing; and sufficient and robust health system. The Philippines scored the lowest in the “health system” (sub-indicator score: 38.2) and “prevention” (38.5) indicators.
A major player in the fight against the pandemic is the Research Institute for Tropical Medicine (RITM). This DOH unit got P519 million in this year’s budget, spearheading the nation’s Covid-19 testing efforts.
Making do
FOR now, the Philippines contends with nearly-13,000 Covid-19 cases, including deaths and recoveries. Over 1,500 health workers have contracted the deadly virus. More than 30,000 overseas Filipino workers, displaced from their host countries and from their ships, have been repatriated.
The hospitals and health facilities in the richer provinces, cities and municipalities not only have more Covid-19 cases; they’re heavily burdened. Contrast this to the burden of developed regions and 42 provinces, like Catanduanes, with no or limited Covid-19 cases.
In the meantime, health facilities in provinces like Catanduanes would have to make do with the support of politicians and private donors.
And the May 11 resolution of the province’s legislative council, a funding window was shut.
Indeed, the country’s health system must rely not on cash but the compassion and profession of professional health workers.
They form the only abundant resource this country has to be strong against the howling winds of Covid-19.