THE COVID-19 pandemic is prompting us to ask: Where are our healthcare workers? Do we have enough?
A study of state think tank Philippine Institute for Development Studies found that healthcare professionals are more likely to work in areas where earnings are potentially high and near communities where they were trained.
According to the study (“Who Are the Health Workers and Where Are They? Revealed Preferences in Location Decision among Health Care Professionals in the Philippines”), the supply of healthcare workers such as nurses, physicians, and midwives are highly uneven in terms of their geographic distribution in the country.
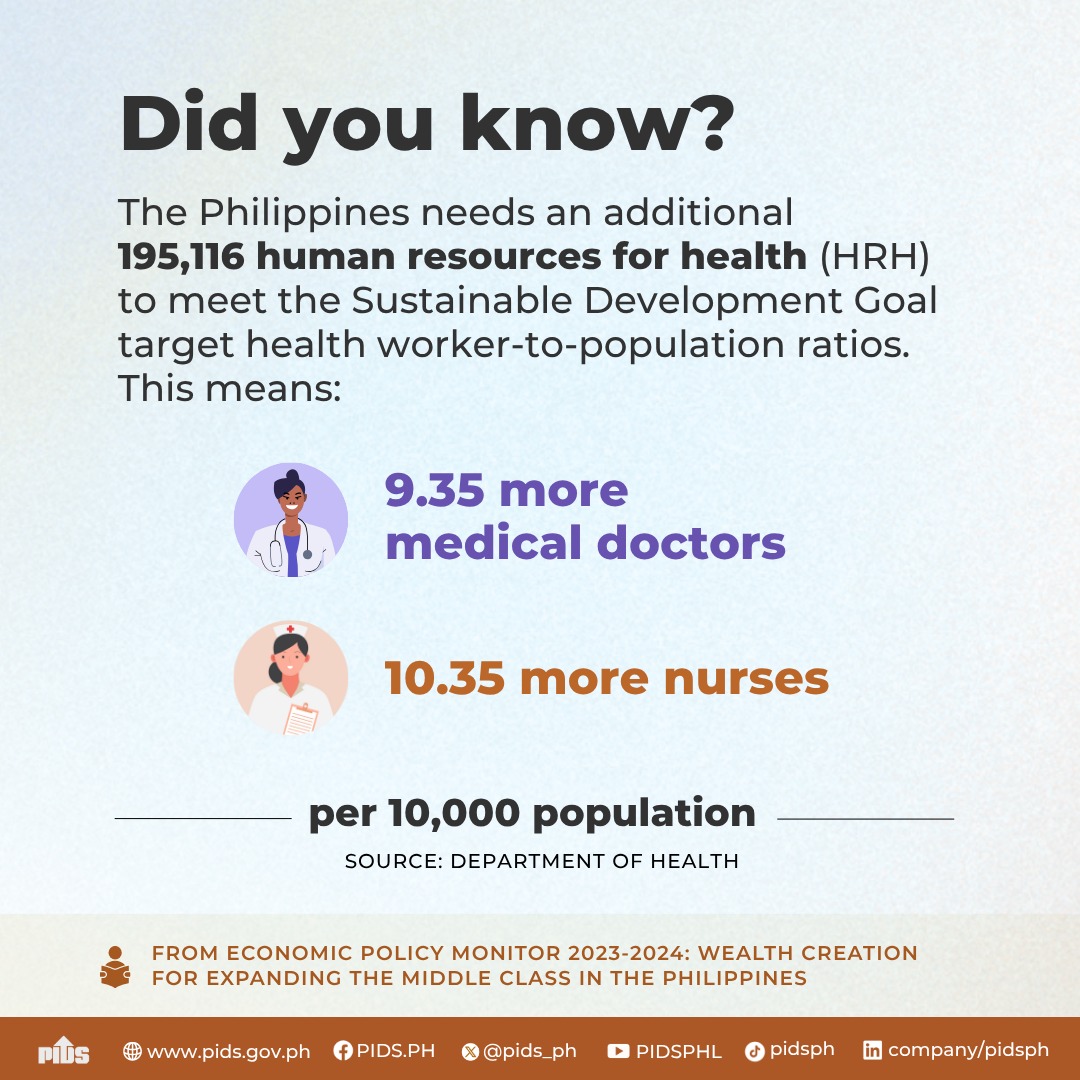
The composite density of physicians, professional nurses, and professional midwives reached 40.8 per 10,000 population in 2015. – above the thresholds set by the World Health Organization (WHO) in 2006 and the International Labour Organization (ILO) in 2011. WHO proposed “a density of 23 skilled health care workers, comprising of physicians, nurses and midwives, per 10,000 population” while the ILO suggested “a density of 34 physicians, nurses and midwives per 10,000 population”. Subsequently, WHO updated its threshold to 45 skilled healthcare workers per 10,000 population in 2016 while ILO updated it to 41 per 10,000 population in 2014.
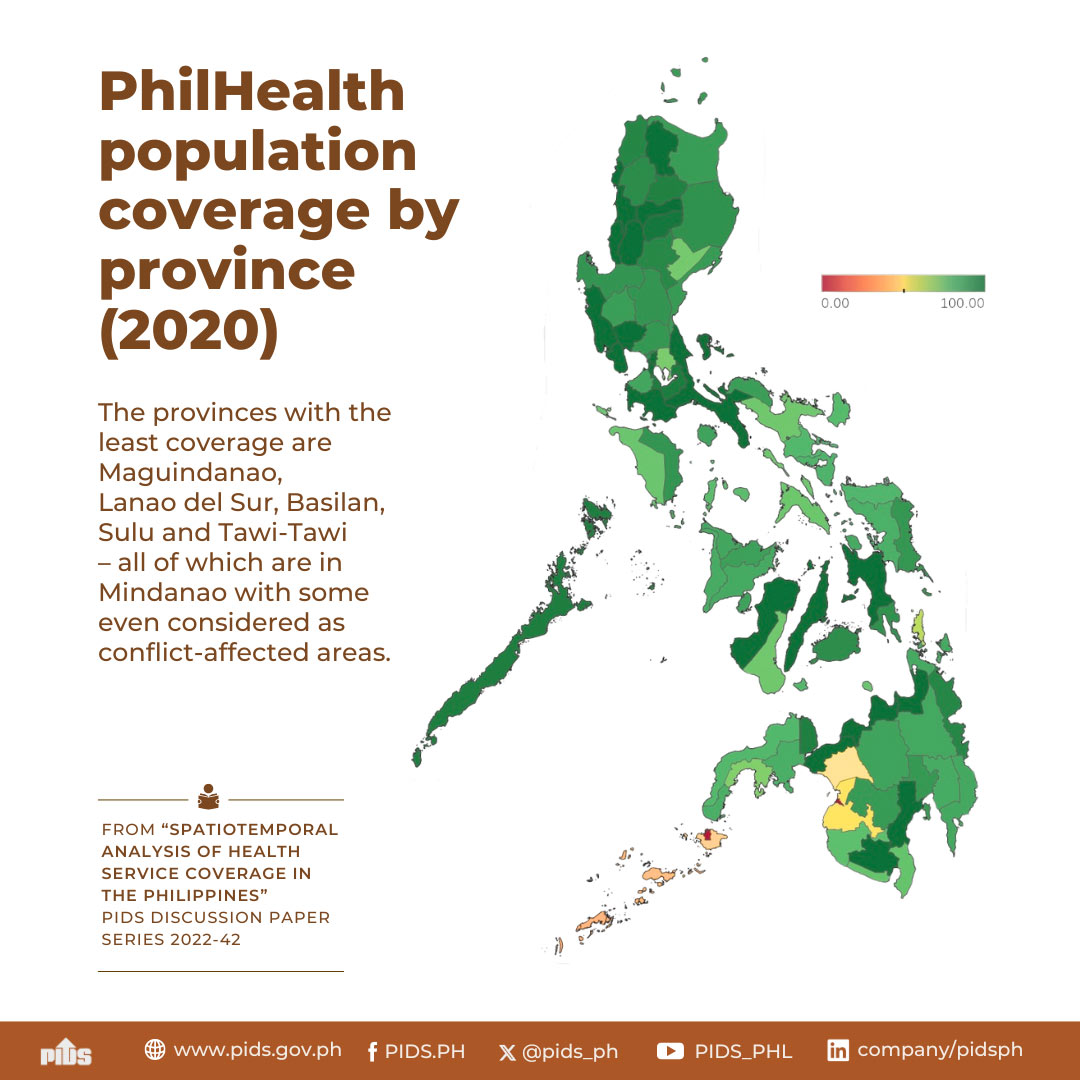
While these international metrics suggest that we have sufficient supply of healthcare workers, the study found out this is not the case based on disaggregated data on health human resource (HHR) density. Less than 25 percent of cities and municipalities have HHR density above the 41 physicians, nurses and midwives per 10,000 population recommended by WHO in 2016. This leaves as much as three-quarters of cities and municipalities in the country with potentially insufficient number of HHRs to provide healthcare services.
The study also found that healthcare professionals are more likely to work in cities and municipalities that have greater access to amenities like hospitals and clinics. However, they are less likely to work in areas with high levels of ethnic concentration.
The continuing maldistribution of healthcare workers can aggravate the country’s problem on limited access to healthcare services. To address this issue, the study bared some policy considerations in designing programs that attract and retain healthcare workers, especially in underserved areas.
One is to boost household incomes through local economic development, which is “essential in ensuring the economic viability of any professional practice, particularly in health care”.
The role of the private sector should also be strengthened in providing healthcare services to the people. Supporting private healthcare practices through the country’s social health insurance system or a similar voucher scheme may provide greater incentives for healthcare workers to practice in underserved areas,
The study also proposed for the reassessment of common- and deep-rooted beliefs on healthcare professional practice. However, it pointed out that “although altruistic motives among healthcare practitioners to serve in rural areas may be important in recruiting HHR for rural practice, it may not necessarily be the most sustainable.”
Is the Health department listening?
A study of state think tank Philippine Institute for Development Studies found that healthcare professionals are more likely to work in areas where earnings are potentially high and near communities where they were trained.
According to the study (“Who Are the Health Workers and Where Are They? Revealed Preferences in Location Decision among Health Care Professionals in the Philippines”), the supply of healthcare workers such as nurses, physicians, and midwives are highly uneven in terms of their geographic distribution in the country.
The composite density of physicians, professional nurses, and professional midwives reached 40.8 per 10,000 population in 2015. – above the thresholds set by the World Health Organization (WHO) in 2006 and the International Labour Organization (ILO) in 2011. WHO proposed “a density of 23 skilled health care workers, comprising of physicians, nurses and midwives, per 10,000 population” while the ILO suggested “a density of 34 physicians, nurses and midwives per 10,000 population”. Subsequently, WHO updated its threshold to 45 skilled healthcare workers per 10,000 population in 2016 while ILO updated it to 41 per 10,000 population in 2014.
While these international metrics suggest that we have sufficient supply of healthcare workers, the study found out this is not the case based on disaggregated data on health human resource (HHR) density. Less than 25 percent of cities and municipalities have HHR density above the 41 physicians, nurses and midwives per 10,000 population recommended by WHO in 2016. This leaves as much as three-quarters of cities and municipalities in the country with potentially insufficient number of HHRs to provide healthcare services.
The study also found that healthcare professionals are more likely to work in cities and municipalities that have greater access to amenities like hospitals and clinics. However, they are less likely to work in areas with high levels of ethnic concentration.
The continuing maldistribution of healthcare workers can aggravate the country’s problem on limited access to healthcare services. To address this issue, the study bared some policy considerations in designing programs that attract and retain healthcare workers, especially in underserved areas.
One is to boost household incomes through local economic development, which is “essential in ensuring the economic viability of any professional practice, particularly in health care”.
The role of the private sector should also be strengthened in providing healthcare services to the people. Supporting private healthcare practices through the country’s social health insurance system or a similar voucher scheme may provide greater incentives for healthcare workers to practice in underserved areas,
The study also proposed for the reassessment of common- and deep-rooted beliefs on healthcare professional practice. However, it pointed out that “although altruistic motives among healthcare practitioners to serve in rural areas may be important in recruiting HHR for rural practice, it may not necessarily be the most sustainable.”
Is the Health department listening?